Dental implant placement and restoration in the esthetic region is one of the most challenging procedures for dental clinicians. We are often faced with bone loss due periodontal disease, trauma, or failed root canal therapy, resulting in inadequate bone width and bone height. Although ideal treatment would be to perform the ridge augmentation necessary to rebuild deficient ridges, this may not always occur. We do our best to explain to patients the necessary steps to achieve great results. And we all know the feeling of having our patients’ enthusiasm wane as we discuss the time and expense involved with bone grafting and gingival grafts necessary to restore these cases properly. In some situations, narrow diameter implants may act as a nice compromise with good results.
Narrow diameter dental implants have a good track record. Five-year studies show a success rate ranging from 91.2% to 96.3%. Narrow diameter dental implants have been gaining in popularity with clinicians as another means to rehabilitate patients with predictable results. Advantages include less invasive surgery, less postop discomfort, and good initial stability, which can make immediate loading possible, preserving and compressing patient’s bone, and conserving the gingival architecture. Cases must be carefully selected. This author believes that bone grafting, gingival grafts, regular diameter and wide diameter implants are all mainstays of implant dentistry; however, via proper case selection, narrow diameter implants are an important addition to our armamentarium.
After thorough clinical examination and careful assessment of a patient’s bone height, width, and gingival architecture and phenotype, we can determine if a narrow diameter implant is a viable option. Bone quality can be determined with a CT scan and/or calipers, and a periodontal probe sounding.
CASE 1
Fig. 1
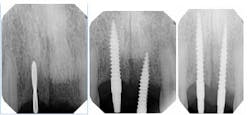
Fig. 2 (Preoperative) 4.5 mm buccal-lingual bone measured with bone calipers.A 1.8 mm pilot drill created the osteotomy for the implant (Fig. 3). In this case, we drilled about 10 mm into the bone and then placed the 3.0 x 16 mm implant afterwards (Fig. 4 and 5). In cases where bone is more dense, the clinician can follow with a 2.5 mm drill to create the osteotomy. The implant abutments were prepped under copious irrigation. The final impression was taken immediately to fabricate a PFM bridge. Since we did not disrupt the blood supply or interrupt the periosteum via flapless surgery, we expect not to have any bone loss or gingival recession following this procedure.
Implant placement 10/20/2011. 1.8 mm pilot drill (left slide). Figs. 3-5 NDI 3.0 x 16 mm implantsLab-fabricated temporaries were relined with acrylic and cemented (Figs. 6 and 7). The patient went through the ordeal of wearing an uncomfortable flipper for 12 years. After only a 45-minute appointment, she was able to smile with implant restorations that she could confidently display. A few weeks later, the final bridge was delivered (Fig. 8). Total clinician time for the entire case was just one hour. Two years later, the case looks exactly the same.
Same day of surgery post implant placement. Fig. 6
Patient left same day with a lab-fabricated temporary bridge. Fig. 7
Final implant bridge delivered on 12/3/2011. Fig. 8
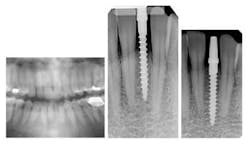
CASE 2This patient was edentulous in the No. 24 and No. 25 area (Fig. 9). She has generalized moderate chronic periodontal disease. Periodontal treatment was performed and patient’s oral hygiene was monitored before implant placement. Because of inadequate bone volume, the case would not allow for traditional implants. 2.5 x 14 mm narrow diameter implants were placed in place of No. 24 and No. 25 (Fig. 10). The patient left the same day with temporaries, and a final bridge was delivered several weeks later (Fig. 11 through 14).
Fig. 9 Initial presentation with missing Nos. 24 and 25
Fig. 10 Dio Secure (narrow diameter dental implants) 2.5 x 14 mm implants
Figs. 11-14 Abutment, temporization, and final restoration
CASE 3This patient had a decayed, mobile primary tooth in the site and No. 24 was deemed restoratively hopeless. The primary tooth was extracted and a 2.5 x 14 mm implant was immediately placed in the extraction socket (Figs. 15 through 18). A temporary was fabricated the same day and loaded (Figs 19 and 20). The site was allowed to heal for eight weeks before taking the final impression (Fig. 21).
Figs. 15-18 Replacing a primary tooth in place of No. 24. Dio 2.5 x 14 mm implant
Figs. 19-21
Conclusion
Thinner dental implants are a viable option in certain cases. Benefits include a less traumatic procedure, immediate loading, avoiding bone and gingival grafts, reduced chairtime, and reduced expense for the patients.