All photos courtesy of Naomi Ramer, DDS Head, neck, and oral squamous cell carcinoma (OSCC) is a disease that is thought to be mostly associated with tobacco use and alcohol consumption. (1) The recent announcement, however, by actor Michael Douglas that his esophageal cancer was caused by oral sex and specifically the human papillomavirus (HPV) has brought nonenvironmental etiologies into the spotlight. In fact, 15% to 20% of OSCCs occur in nonsmokers and nondrinkers, suggesting the presence of other risk factors. Recent studies suggest that HPV infections of the upper respiratory area may lead to head and neck tumors. (2) In the cases like Michael Douglas, some experts estimate that about 14,000 throat cancers are diagnosed every year in the United States, and about 70% of those are related to HPV. (3) In one study,HPV presence in the oral cavity was associated with increased risk of oral cavity or oropharyngeal cancer (odds 3.7 with a 95% confidence interval), independent of alcohol and tobacco exposure. (4) Men with cancers at these sites also had sexual risk factors similar to those for women with cervical cancer associated with HPV infections, such as early age of first intercourse, multiple sexual partners, and a history of genital warts.
ADDITIONAL READING: Before you look at the teeth, look at this: our responsibility to detect and treat oral cancer
HPV is a double-stranded DNA virus that infects the epithelial cells of skin and mucosa. Epithelium, comprised of a certain type of cell (squamous cells) line the skin and/or mucosa of the mouth, throat, tongue, tonsils, vagina, cervix, vulva, urethra, and anus. Transmission of the virus occurs when these areas come into contact with a virus, allowing it to transfer between epithelial cells.ADDITIONAL READING: Seriously, how meticulously do you check for oral cancer?
The HPV family contains almost 200 strains, and it is one of the most common viruses in the United States. Out of all of the 200 strains of HPV, only nine are associated with cancers. Of the nine that are high risk, only one is strongly associated with oropharyngeal cancer, HPV 16. Many studies suggest that seropositivity to HPV 16 capsid protein is significantly greater in oral cancer patients than in control subjects. (5)
ADDITIONAL READING: Head, neck, and oral cancer: A general reference for treatment
The problem of HPV is that infections are widespread and often do not cause symptoms, so the host does not know he or she is infected. The CDC estimates that up to 80% of Americans will have HPV infections in their lifetime and 99% will clear these infections not knowing that they had the infection, as it produces no symptoms.
So what can you do as a dental professional? Knowledge is key and a proper oral cancer screening can make great strides in the fight against oral cancer. Census data estimates that there are more than 100,000 dentists in the United States, each one seeing between eight and 15 patients per day. However, published studies show that currently fewer than 25% of those patients who visit a dentist regularly report having had an oral cancer screening.
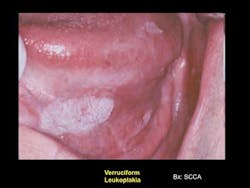
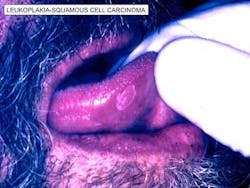
A proper oral cancer screening should consist of a systematic visual examination of all the soft tissues of the mouth, including manual extension of the tongue to examine its base, a bimanual palpation of the floor of the mouth, a digital examination of the borders of the tongue, and the lymph nodes surrounding the oral cavity and in the neck. (6) Detailed discussion of sexual activity including oral sex history should take place to identify high-risk individuals especially since HPV 16-associated oral cancers are on the rise. Adjuncts to the visual exam such as dyes, lights, and brush biopsy kits can be used in conjunction with visual and tactile exams.
Once suspect tissues have been detected, the only way a definitive diagnosis of oral cancer may be made is through biopsy. Any condition that has existed for 14 days or more without resolution should be considered suspect and worthy of further diagnostic procedures or referral. If an area doesn’t resolve in two weeks, one can rule out the two most prevalent lesions that often appear, such as oral cancer herpes simplex ulcerations and apthous ulcers.
References
1. Mashberg A, Boffetta P, Winkelman R, Garfinkel L. Tobacco smoking, alcohol drinking, and cancer of the oral cavity and oropharynx among U.S. veterans. Cancer. 1993;72:1369-1375.
2. Gillison M, Koch WM, Shah KV. Human papillomavirus and head and neck squamous cell carcinoma: are some head and neck cancers sexually transmitted disease? Curr Opin Oncol. 1999;11:191-199.
3. http://www.boston.com/2011/10/25/hpv/qvTAFdC9mmEJLGUZUCcC2I/story.html
4. Schwartz SM, Daling JR, Doody DR, Wipf GC, Carter JJ, Madeleine MM,et al. Oral cancer risk in relation to sexual history and evidence of human papillomavirus infection. J Natl Cancer Inst. 1998;90:1626-1636.
5. Smith EM, Hoffman HT, Summersgill KS, Kirchner HL, Turek LP, Haugen TH. Human papillomavirus and risk of oral cancer. Laryngoscope. 1998;108:1098-1103.
6. http://www.oralcancerfoundation.org/dental/role_of_dentists.php