Socket debridement paresthesia: A popular method of unintentionally making a patient numb after tooth extraction
The incidence of overall paresthesia after tooth extraction is on the rise due to increasing numbers of extractions over the years. Injuries to the inferior alveolar nerve and lingual nerve can cause problems with speech and mastication, leading to complaints and possible litigation as these injuries begin to affect patients' quality of life. Dr. Scott Froum reviews one iatrogenic cause of mandibular nerve injury post tooth extraction and offers prevention strategies.
Although the complication rate of tooth extraction is low, and complications that do occur are often minor, the incidence of overall paresthesia post tooth extraction is on the rise due to an increase in the number of teeth being extracted over the years. In the mandible, teeth that are especially close in proximity to the lingual, inferior alveolar, mylohyoid, and buccal nerves run the greatest chance of developing nerve impairment post extraction. Most studies have shown that if the paresthesia follows extraction, it is likely to be temporary and resolve within the first six to eight weeks after the trauma, although it may take up to 24 months.
If paresthesia is not completely resolved within about two months, the probability of a permanent deficit increases significantly. (1) However, if no improvement is seen after two years of follow-up, the altered sensation is likely to represent nerve dysfunction that may be in the form of permanent neurosensory disability, a complete loss of sensory function, and neurogenic symptoms. (2) Injuries to the inferior alveolar nerve (IAN) and lingual nerve can be particularly troublesome, causing problems with speech and mastication, possibly adversely affecting the patient’s quality of life. Such nerve injuries also constitute one of the most frequent causes of complaints and litigation. This article will review one iatrogenic cause of mandibular nerve injury after tooth extraction and explain steps the dentist can take to prevent such injuries in the future.
The mandibular nerve is the third and most inferior branch of the trigeminal nerve (fifth cranial nerve). The nerve enters the mandible through the mandibular foramen on the medial surface of the ascending mandibular ramus. After passing through the mandibular foramen, the nerve is called the inferior alveolar nerve (IAN). In the molar region, the IAN divides into the mental and mandibular incisal nerves. The frequency of mandibular nerve injury (inferior alveolar nerve injury) is relatively low, but it increases as the roots of the tooth move closer to the inferior alveolar nerve. (3)
The best method of preventing nerve injury is to be prepared and evaluate nerve anatomy prior to the procedure on panoramic radiography and CT scans. (4) Several techniques have been described to reduce the risk of nerve injury during tooth extraction when the tooth-nerve is in proximity. Orthodontic extrusion, (5) surgical sectioning, (6) and induced spontaneous eruption (7) are all well covered in the literature. However, there seems to be a lack of discussion in the literature regarding the incidence of iatrogenic nerve injury due to socket debridement post tooth extraction.
Aggressively debriding granulation/cystic tissue after tooth extraction is important for the removal of bacteria, inducing angiogenesis, and the promotion of the blood clot. This is especially true when subsequent grating and dental implants are in the treatment plan. The importance of thorough socket debridement should be second to inducing a transient or permanent injury via instrument penetration into the nerve space. According to Oral Surgeon Gregg Jacob, DMD, even if large lesions are present (figure 1), “Leaving granulation tissue and allowing the body to resorb pathology is more prudent than risking nerve injury.”
Figure 1: Large periapical area near the IAN prior to tooth extraction
In many cases, removing these lesions in their entirety will increase the risk of canal penetration (figure 2) and subsequent paresthesia (figure 3).
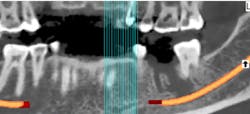
Figure 2: CT scan showing penetration of IAN canal after extraction and socket debridement
Figure 3: Area of resulting paresthesia mapped out clinically
MORE FROM DR. SCOTT FROUM |Postextraction treatment: Did your bone graft fail, or did you fail your bone graft?
The lack of a definitive answer in the literature between which of these two socket debridement methodologies to follow—complete debridement versus leaving granulation tissue—suggests that a combination approach may be a wise choice when there are nerve considerations.
In summation, the best treatment for nerve injury continues to be prevention. If there is any doubt by the treating clinician as to the proximity of an odontogenic lesion to the nerve space (figure 4), a CT scan prior to extraction therapy is the gold standard of care (figure 5). This pretreatment diagnostic can avoid both clinical and legal headaches.
Figure 4: Another case demonstrating periapical pathology and its proximity to the IAN
Figure 5: Preoperative CT scan obtained prior to tooth extraction to prepare for surgery and limit the possibility of nerve violation
MORE CLINICAL TIPS FROM DR. SCOTT FROUM . . .
References
1. Robinson PP. Observations on the recovery of sensation following inferior alveolar nerve injuries. Br J Oral Maxillofac Surg. 1988;26(3):177-189.
2. Wofford DT, Miller RI. Prospective study of dysesthesia following odontectomy of impacted mandibular third molars. J Oral Maxillofac Surg. 1987;45(1):15-19.
3. Bui CH, Seldin EB, Dodson TB. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. 2003;61(12):1379-1389.
4. Tantanapornkul W, Okouchi K, Fujiwara Y et al. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(2):253-259. Epub 2006 Sep 1.
5. Wang Y, He D, Yang C, Wang B, Qian W. An easy way to apply orthodontic extraction for impacted lower third molar compressing to the inferior alveolar nerve. J Craniomaxillofac Surg. 2012;40(3):234-237. doi: 10.1016/j.jcms.2011.05.001.
6. Dolanmaz D, Yildirim G, Isik K, Kucuk K, Ozturk A. A preferable technique for protecting the inferior alveolar nerve: coronectomy. J Oral Maxillofac Surg. 2009;67(6):1234-1238. doi: 10.1016/j.joms.2008.12.031.
7. Landi L, Manicone PF, Piccinelli S, Raia A, Raia R. A novel surgical approach to impacted mandibular third molars to reduce the risk of paresthesia: a case series. J Oral Maxillofac Surg. 2010;68(5):969-974. doi: 10.1016/j.joms.2009.09.097.