Avoiding dental implants and the sinus lift procedure: Revisiting maxillary molar root amputation
The replacement of hopeless or missing teeth can be predictably achieved with dental implants and have historically high survival rates.1 Implants placed in the mandible have demonstrated higher survival rates than implants placed in the maxilla,2 but if performed correctly maxillary implants still enjoy high survival rates in the literature.3,4
Implant failures do occur, however, and implants placed in the posterior maxilla typically have the highest chance of failure.5 Reasons for increased implantRoot amputation: How and why?
Case selection and clinical considerations
Saving compromised multirooted teeth with root amputation can often be successful, but the technique is sensitive and complex. Proper case selection is essential, and considerations include the following:
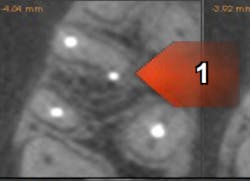
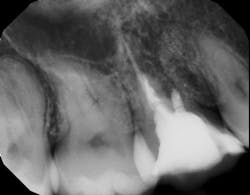
There is sufficient bone support around the remaining roots (at least 50% or more is needed) along with sufficient coronal tooth structure (figure 3).How does root amputation compare with other surgical procedures?
The prognosis is good for molar teeth treated with root amputation, provided case selection and treatment are performed properly. Fugazzottoreported 15-year cumulative success rates comparing molar root resection to molar implant placement, with survival rates of 96.8% for root-resected molars and 97.0% for molar implants.10 This study was done in private practice with proper oversight and case selection.Conclusion
Root amputation remains a viable treatment to save maxillary molars and can have long-term success rates equal to dental implant therapy (figures 9 and 10).Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- Brånemark PI, Hansson BO, Adell R, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl. 1977;16:1-132.
- Fouda AAH. The impact of the alveolar bone sites on early implant failure: a systematic review with meta-analysis. J Korean Assoc Oral Maxillofac Surg. 2020;46(3):162-173. doi:10.5125/jkaoms.2020.46.3.162
- den Hartog L, Slater JJRH, Vissink A, Meijer HJA, Raghoebar GM. Treatment outcome of immediate, early and conventional single-tooth implants in the aesthetic zone: a systematic review to survival, bone level, soft-tissue, aesthetics and patient satisfaction. Clin Periodontol. 2008;35(12):1073-1086. doi:10.1111/j.1600-051X.2008.01330.x
- Adell R, Lekholm U, Rockler B, Brånemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg. 1981;10(6):387-416. doi:10.1016/s0300-9785(81)80077-4
- Pabst AM, Walter C, Ehbauer S, et al. Analysis of implant-failure predictors in the posterior maxilla: a retrospective study of 1395 implants. J Craniomaxillofac Surg. 2015;43(3):414-420. doi:10.1016/j.jcms.2015.01.004
- Huynh-Ba G, Friedberg JR, Vogiatzi D, Ioannidou E. Implant failure predictors in the posterior maxilla: a retrospective study of 273 consecutive implants. J Periodontol. 2008;79(12):2256-2261. doi:10.1902/jop.2008.070602
- Kasat V, Ladda R. Smoking and dental implants. J Int Soc Prev Community Dent. 2012;2(2):38-41. doi:10.4103/2231-0762.109358
- Walter C, Weiger R, Zitzmann NU. Periodontal surgery in furcation-involved maxillary molars revisited—an introduction of guidelines for comprehensive treatment. Clin Oral Investig. 2011;15(1):9-20. doi:10.1007/s00784-010-0431-9
- Park SY, Shin SY, Yang SM, Kye SB. Factors influencing the outcome of root-resection therapy in molars: a 10-year retrospective study. J Periodontol. 2009;80(1):32-40. doi:10.1902/jop.2009.080316
- Fugazzotto PA. A comparison of the success of root resected molars and molar position implants in function in a private practice: results of up to 15-plus years. J Periodontol. 2001;72(8):1113-1123. doi:10.1902/jop.2001.72.8.1113
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a PhD candidate in the field of functional and integrative nutrition. Contact him through his website at drscottfroum.com or (212) 751-8530.