Postextraction treatment: Did your bone graft fail, or did you fail your bone graft?
If patients are about to undergo a dental treatment, especially surgery, they often will inquire as to the success rate of the procedure to be performed. When a tooth is diagnosed as being hopeless and extraction is warranted, the success rates of tooth extraction without subsequent infection are high. (1) One systematic review suggested that this rate of infection is further decreased with the use of prophylactic antibiotics and/or post-treatment antibiotics. (2) In addition, the literature suggests that tooth extraction procedures followed by bone-graft replacement for the purposes of implant site preservation also enjoy high success rates. (3) However, like every other procedure in dental medicine, failures do occur. When we look at the etiology of poor bone fill or bone-graft integration postextraction, there are many factors that influence outcome, including medical history (immune disorders), medications (bisphosphonates), social factors (smoking), etc. There are also iatrogenic factors, including sterility of the procedure, surgical technique, and—one of the most important and often-overlooked factors—completedebridement of the postextraction socket.
ADDITIONAL READING |Does your dental extraction socket need a bone graft: A decision matrix
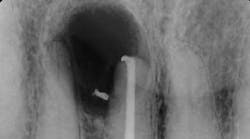
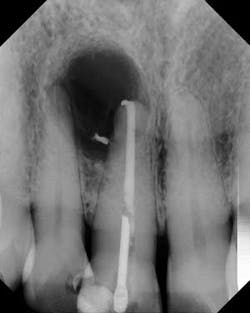
Although the literature varies as to the amount of bone volume that can be created/preserved, what material to use, as well as the indications for these procedures, (4) the majority of these studies agree that socket debridement is essential post-tooth extraction to ensure a good result. Socket debridement is particularly important when acute/chronic infections are present and cystic material lines the alveolar socket and/or tooth (figures 1 and 2). The complete removal of this infected tissue (figure 3) is tantamount to good bone fill, and can be the source of bone-graft contamination and infection.
After removal of the tooth, there are many methods of debriding the socket and various instrumentation that one can use. This author chooses to use a spoon excavator or spoon curette with serrations as a means of performing mechanical debridement (figure 4). After mechanical debridement, copious saline is used to irrigate the socket (figure 5), followed by the placement of cotton pellets soaked with either tetracycline (50 mg/ml) or 60% citric acid into the socket. After chemical modification, the socket is again irrigated and flushed with saline.
ADDITIONAL READING |Manage, repair, or regenerate periodontal disease?
Visual inspection of the socket postdebridement should show a clean alveolus with no evidence of fibrous tissue tags (figure 6). Although irrigation and decontamination are important, equally important is to ensure that the socket is not desiccated by these procedures. Studies have shown that poor bone healing and dry sockets have occurred postsocket irrigation if bleeding is not stimulated. (5) Decortication of the socket to initiate blood flow is recommended prior to bone grafting/socket closure to initiate osteoinduction/angiogenesis and clot formation (figure 7). By creating the right environment for bone healing and removing obstacles to maturation, your bone graft will appreciate your efforts and reward you with good integration and healing.
MORE CLINICAL TIPS FROM DR. SCOTT FROUM . . .
References
1. Bui CH, et al. Types, frequencies, and risk factors for complications after third molar extraction. J Oral Maxillofac Surg. 2003;61:1379–1389.
2. Lodi G, Figini L, Sardella A, Carrassi A, Del Fabbro M, Furness S. Antibiotics to prevent complications following tooth extractions. Cochrane Database of Systematic Reviews. 2012;(1).
3. Carmagnola D, Adriaens P, Berglundh T. Healing of human extraction sockets filled with Bio-Oss. Clin Oral Implants Res. 2003;14(2):137–43.
4. Froum SJ, Wallace SS, Elian N, et al. Comparison of mineralized cancellous bone allograft (Puros) and anorganic bovine bone matrix (Bio-Oss) for sinus augmentation: histomorphometry at 26 to 32 weeks after grafting. Int J Periodontics Restorative Dent. 2006;26(6):543–551.
5. Tolstunov L, et al. Influence of immediate post-extraction socket irrigation on development of alveolar osteitis after mandibular third molar removal: a prospective split-mouth study, preliminary report. Brit Dent Journal. 2012;213(12): 597–601.
Scott Froum, DDS, is a periodontist in private practice in New York City. He is the editorial director of Perio-Implant Advisory e-newsletter, as well as a contributing author for DentistryIQ and Dental Economics. Dr. Froum is a clinical associate professor at the New York University Dental School in the Department of Periodontology and Implantology, and a diplomate of the American Board of Periodontology. Contact him through his website at drscottfroum.com.