Halitosis: Detecting bad breath using oral chromatography
Halitosis, commonly known as bad breath, is a condition that affects a significant portion of the population across all ages, backgrounds, and cultures. Most people have experienced halitosis that comes and goes or occurs after eating certain foods like onions or garlic. Transient halitosis can typically be resolved by improving oral hygiene practices. But for some, halitosis is a chronic condition that can lead to social embarrassment, difficulty maintaining relationships, and poor self-esteem.
While the origin of chronic halitosis can be limited to the oral cavity, there are many extraoral factors that contribute to this condition, such as medications, gastrointestinal dysfunction, and other metabolic disorders. Due to the multifactorial nature of halitosis, many people who suffer from chronic halitosis have difficulty obtaining effective treatment and are oftentimes left without answers. In this article, we will discuss using oral chromatography as a key diagnostic tool in the detection, quantification, and treatment of halitosis.
Sulfur compounds are responsible for bad breath
The gases emanating from the mouth that cause oral malodor are the volatile sulfur compounds (VSCs).1 When organic substrates—such as sulfur-containing peptides, amino acids in saliva, gingival crevicular fluid, blood, and desquamated epithelial cells—are broken down, VSCs are produced.2 The VSCs created in the oral cavity during this degradation process include hydrogen sulfide, methyl mercaptan, and dimethyl sulfide. These three VSCs are considered to be the most important contributors to breath malodor, and thereby provide an appropriate biomarker for breath quality evaluation.3
What is oral chromatography?
When halitosis is suspected despite satisfactory oral hygiene and the absence of periodontal disease and dental caries, we must use a more precise diagnostic approach. Oral chromatography is a specific type of gas chromatography used to measure VSCs. By using oral chromatography, we are not only able to determine the presence of VSCs, but also the concentration of each gas.
The method for collecting a gas sample from each patient differs slightly from one oral chromatography device to another. One method used to collect a breath sample is with a plastic syringe. The syringe is positioned in the patient’s mouth until the flange of the syringe reaches the patient’s lips (figure 1). The patient is instructed to breathe through their nose while keeping the oral cavity sealed and unventilated for 30 seconds. After a series of breaths from the patient, a sample is collected in the syringe and injected into the OralChroma for analysis.
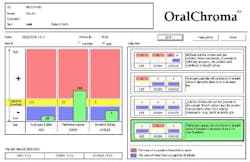
Once the gas sample is analyzed by the OralChroma, the results appear as shown in Figure 2. For each of the three VSCs—hydrogen sulfide (H2S), methyl mercaptan (CH3SH), and dimethyl sulfide ([CH3]2S)—there is a cognitive threshold unique to each gas (112 ppb, 26 ppb, and 8 ppb, respectively). The results appear as an easy-to-read visual showing the concentration of each gas in parts per billion (ppb) and if that gas is at, above, or below human capability of detection.
Steps following a positive oral chromatography result
If an oral chromatography reveals the patient is above the cognitive threshold in one or more VSCs, a BiofilmDNA test is indicated. Using qPCR, a BiofilmDNA test detects various oral microorganisms present in the oral cavity. The whole-mouth BiofilmDNA analysis offers a comprehensive analysis and risk assessment of eight tested pathogens. Pathogens responsible for periodontal disease include A. actinomycetemcomitans, F. nucleatum, P. micros, T. denticola, T. forsythia, and P. gingivalis. Cariogenic risk is determined by the S. mutans population. Oral yeast risk is determined by the C. albicans population.
After an assessment of a patient’s oral pathogens, VSCs, and an in-depth patient history, practitioners can begin to determine how to appropriately treat halitosis for each patient. If it is suspected that the origin of halitosis is beyond the oral cavity, functional gastrointestinal testing may be indicated to evaluate the overall health and function of the gut.
The gut microbiome can be analyzed using a sample of the patient’s stool, urine, saliva, or dried blood spot. Depending on the specific test, one or more samples may be needed for analysis. Functional wellness testing provides information about the diversity of the gut microbiome, fungal imbalances, digestive function, nutrient absorption, GI motility, gut inflammation, immune function, intestinal permeability, and gut barrier function.4 A summary of test results shown in Figure 3 gives patients a visual to understand the level of support needed in each category of gut health.
Once testing is reviewed with the patient, the practitioner can create an individualized series of treatment that aims to detoxify, repair, and rebalance the gut microbiome, and ultimately treat the underlying cause of halitosis.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- Tungare S, Zafar N, Paranjpe AG. Halitosis. In: StatPearls [Internet]. StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/books/NBK534859/
- Sinjari B, Murmura G, Caputi S, Ricci L, Varvara G, Scarano A. Use of Oral Chroma in the assessment of volatile sulfur compounds in patients with fixed prostheses. Int J Immunopathol Pharmacol. 2013;26(3):691-697. doi:10.1177/039463201302600312
- Snel J, Burgering M, Smit B, et al. Volatile sulphur compounds in morning breath of human volunteers. Arch Oral Biol. 2011;56(1):29-34. doi:10.1016/j.archoralbio.2010.08.016
- GI Spotlight test from designsforhealth.com
About the Author

Gianna Pico, DMD
Gianna Pico, DMD, is a general dentist practicing in New York and New Jersey. She received her BS from Boston College, MS in oral health sciences from Boston University, and DMD from Boston University Henry M. Goldman School of Dental Medicine, graduating with honors. She continued her dental training back in her home state of New York at Interfaith Medical Center where she completed a general practice residency. Dr. Pico is motivated to provide customized and patient-centric care with a true emphasis on the oral-systemic connection.

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.