Increase in oral dysplasia and oral cancer rates due to COVID-19 alcohol-related consumption
The COVID-19 pandemic has profoundly affected all aspects of life, including health. One of the more concerning developments is the increase in oral cancer rates because of greater alcohol consumption during this period. Research indicates that, due to financial insecurity, depression, general anxiety, and boredom surrounding the pandemic, people turned to risky behavior, most notably alcohol use, in order to cope with their increase in stress.1
Alcohol use during the COVID-19 pandemic
One study showed that although smoking rates dropped 1.1% from 15.3% to 14.2% among those aged 18-54, rates increased slightly in individuals over the age of 55.2 Alcohol use, on the other hand, increased dramatically in all age groups. In 2020, the first year of the pandemic, sales of alcohol increased by 2.9%, the largest annual increase in more than 50 years.3
Another study found alcohol-related deaths increased by 2.2% in the past 20 years prior to the pandemic, and then suddenly jumped 25.5% between 2019 and 2020, totaling 99,107 deaths.4 This same study showed alcohol-synthetic opioid-related deaths jumped a staggering 59.2% among people aged 25-44 during the pandemic.
In addition to deaths, pandemic-related increases in alcohol consumption have been associated with other negative health outcomes, such as increases in transplants for alcohol-associated liver disease,5 emergency department visits for alcohol withdrawal and excess consumption,6 as well as an increase in oral dysplasia and oral cancer diagnosis.
You may also be interested in …
Alcohol and oral cancer: Quantities and effects
Predicting health decline in our patients: A simple test dental professionals can perform
Alcohol use and oral cancer
The link between oral cancer and alcohol consumption is well-documented in the literature. Studies have shown that moderate alcohol consumption (two to four drinks per day) can increase the risk of oral cancer by 1.4 times that of a nondrinker. Heavy alcohol consumption (more than five drinks per day or 15 drinks per week) can increase the risk of oral cancer by 5 times that of a nondrinker.7 This risk is further exacerbated when alcohol is combined with tobacco use and smoking.8
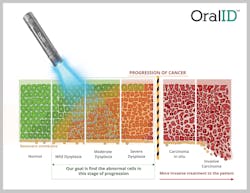
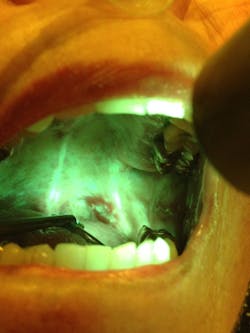
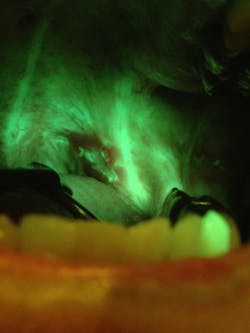
OralID and biopsy to diagnose oral dysplasia
In this study, the author and colleagues identified 53 suspicious lesions (figure 1) in the oral cavity through the use of handheld autofluorescence technology (OralID). The lesions were then sent for biopsy during the period of 2021-2023. The lesions were histochemically stained and sectioned, and graded according to dysplastic progression (figures 2a-2d). Sixty-four percent of the specimens biopsied returned with a grade of mild to moderate epithelial dysplasia or higher.
For example, records at one of the oral pathology clinics used in this study showed that in the three years prior to the COVID-19 pandemic, 17.6% of specimens submitted for biopsy showed precancerous lesions. In the years post–COVID-19, that number rose to 47%. When questioned during the medical intake, 68% of the study’s subjects admitted to increasing their use of alcohol during the pandemic years.
This dramatic rise in dysplastic progression prompted the authors to write this article and call attention to this growing problem in dental health. According to Dr. Naomi Ramer:
Prior to COVID, specimens submitted to the oral pathology laboratory rarely were accompanied with clinical data on alcoholism alone. In 2021, we began seeing an increased number of biopsies submitted on patients with suspicious clinical lesions and a history of significant alcohol intake, or heavy drinkers. The clinical lesions are precancerous leukoplakias and or erythroplakias. When analyzed microscopically, results showed varying degrees of precancerous epithelial dysplasia, epithelial hyperplasia, hyperkeratosis, and frank carcinomas.
These sentiments were echoed in a recent paper published in the Journal of the American Dental Association that called for more diligent approaches to oral cancer screenings because of a rise in risk factors associated with oral cancer due to the COVID-19 pandemic. The article states that in addition to interrupting the continuity of dental care and preventive dental care visits, the pandemic led to increases in certain risk factors for oral carcinogenesis, including increased use of tobacco and alcohol, poor diet, and increased rates of obesity and poor oral hygiene.9
Conclusion
Overall, the COVID-19 pandemic has had a profound impact on our health and well-being. One direct effect of this is an increase in oral cancer rates due to the increase in alcohol consumption due to pandemic-related anxiety and stress. Dental care affiliates must be aware, vigilant, and screen patients (whenever possible) for suspicious oral lesions. OralID autofluorescence technology provides a quick and noninvasive method to increase oral cancer screening that can be employed by the dentist and hygienist during routine exams.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- Rodriguez LM, Litt DM, Stewart SH. Drinking to cope with the pandemic: the unique associations of COVID-19-related perceived threat and psychological distress to drinking behaviors in American men and women. Addict Behav. 2020;110:106532. doi:10.1016/j.addbeh.2020.106532
- Gaffney A, Himmelstein DU, Woolhandler S. Smoking prevalence during the COVID-19 pandemic in the United States. Ann Am Thorac Soc. 2022;19(6):1065-1068. doi:10.1513/AnnalsATS.202110-1184RL
- Slater ME, Alpert HF. Surveillance report #119. Apparent per capita alcohol consumption: national, state, and regional trends, 1977-2020. National Institute on Alcohol Abuse and Alcoholism. Division of Epidemiology and Prevention Research. April 2022. https://pubs.niaaa.nih.gov/publications/ surveillance119/surveillance-report119.pdf
- White AM, Castle IJP, Powell PA, Hingson RW, Koob GF. Alcohol-related deaths during the COVID-19 pandemic. JAMA. 2022;327(17):1704-1706. doi:10.1001/jama.2022.4308
- Cholankeril G, Goli K, Rana A, et al. Impact of COVID-19 pandemic on liver transplantation and alcohol-associated liver disease in the USA. Hepatology. 2021;74(6):3316-3329. doi:10.1002/hep.32067
- Esser MB, Idaikkadar N, Kite-Powell A, Thomas C, Greenlund KJ. Trends in emergency department visits related to acute alcohol consumption before and during the COVID-19 pandemic in the United States, 2018-2020. Drug Alcohol Depend Rep. 2022;3:100049. doi:10.1016/j.dadr.2022.100049
- LoConte NK, Brewster AM, Kaur JS, Merrill JK, Alberg AJ. Alcohol and cancer: a statement of the American Society of Clinical Oncology. J Clin Oncol. 2018;36(1):83-93. doi:10.1200/JCO.2017.76.1155
- Hashibe M, Brennan P, Chuang SC, et al. Interaction between tobacco and alcohol use and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Cancer Epidemiol Biomarkers Prev. 2009;18(2):541-550. doi:10.1158/1055-9965.EPI-08-0347
- Nath S, Ferreira J, McVicar A, Oshilaja T, Swann B. Rise in oral cancer risk factors associated with the COVID-19 pandemic mandates a more diligent approach to oral cancer screening and treatment. J Am Dent Assoc. 2022;153(6):495-499. doi:10.1016/j.adaj.2022.01.001
Naomi Ramer, DDS, is a native of metropolitan New York, where she is currently associate professor of pathology and dentistry and director of oral pathology at Mount Sinai Hospital. She is also the program director for their CODA-accredited oral and maxillofacial pathology residency program. She is a graduate of the New York University College of Dentistry. Dr. Ramer is an author of many publications and book chapters, as well as a presenter at numerous professional symposia. In 2005 she began a long-standing research project on adenoid cystic carcinoma.