coauthor: Don Rothenberg
Short implants may seem to be an obvious alternative where conventional implants are not an option without additional surgical procedures to compensate for tissue deficiencies in posterior regions. However, the question remains: Are survival rates for short implants the same as conventional dental implants? Dr. Scott Froum and Don Rothenberg discuss the benefits of using short implants in certain situations as a method to avoid having to do more invasive grafting.
ALTHOUGH DENTAL IMPLANTS have enjoyed a high survival rate in the literature, failures do occur. (1) Implants placed in the posterior region have been associated with higher failure rates due to biologic limitations, such as less available bone height and poorer bone quality than in anterior regions. (2) In addition, restored teeth in posterior regions usually experience higher occlusal loads than their anterior counterparts. (3) Anatomical structures, such as the maxillary sinus or inferior alveolar nerve canal, may limit the length of the dental implant in the posterior region.
Surgical procedures to compensate for this tissue deficiency—such as lateral window sinus augmentation, transcrestal sinus elevation, and/or guided bone ridge augmentation procedures—have proven to be successful in providing sufficient bone quantity and quality for implant placement and prosthetic support. (4) These procedures, however, prolong the time to final restoration, increase surgical involvement, increase morbidity, and substantially increase treatment expense. (5)
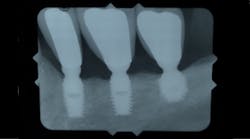
Alternatives to performing these additional augmentation procedures in cases where patients have atrophic posterior regions have come in the form of shortened implants (figures 1 and 1a). Short implants have been defined in the literature as implant lengths that are less than 10 mm. (6) Although the use of short implants seems to be an obvious alternative in cases where conventional implants are not an option without additional procedures, the question is: Do short implants have the same survival rates as conventional-length implants? The answer has been mixed in the historical literature. (7)
Figure 1: Short implants placed more than 20 years ago to avoid inferior alveolar nerve
Figure 1a: Short implant placed more than 10 years ago to avoid maxillary sinus
The most recent study on short dental implants involved a randomized clinical trial evaluating single-tooth short implants (6 mm) versus conventional implants (10 mm) over a five-year period. (8) Survival rates and crestal bone loss around the implant were the primary endpoints in this study. The study also looked at crown-to-implant ratio and tried to determine if that played any role in survival rates.
At the end of five years, 6-mm implants showed a 91% survival rate compared with a 100% survival rate of the 10-mm implants. Marginal bone loss was no different between the 6-mm and 10-mm implants. In addition, average crown-to-implant ratio for the 6-mm implants was 1.75:1 versus 1:1 with the 10-mm implants. These ratios did not affect bone loss. The results of this study would suggest that in areas of limited bone volume and/or height, short dental implants can save T-I-M-E.
4 ways short dental implants can save T-I-M-E:
1. Time: Typical healing periods after sinus and ridge augmentation procedures can range from six to nine months, significantly increasing the time a patient needs to wait for crown restoration.
2. Involvement: Although technology has improved the degree of surgical invasiveness associated with augmentation procedures, short implants decrease the surgical time needed for implant placement.
3. Morbidity: Augmentation procedures, especially those involving split-thickness flap dissection, increase the patient’s likelihood of morbidity—such as swelling, bruising, inflammation, and pain—compared with short dental implants (figure 2).
4. Expense: Because augmentation procedures require more surgical time, graft materials, and office visits, there can be a significant increase in treatment costs for the patient as compared with placement of short dental implants alone.
Figure 2: Extensive swelling after maxillary sinus augmentation
References
1. Zitzmann NU, Berglundh T. Definition and prevalence of peri‐implant diseases. J Clin Periodontol. 2008;35(suppl 8):286-291. doi: 10.1111/j.1600-051X.2008.01274.x.
2. Roos‐Jansåker AM, Renvert H, Lindahl C, Renvert S. Nine‐ to 14‐year follow‐up of implant treatment. Part III: factors associated with peri‐implant lesions. J Clin Periodontol. 2006;33(4):296-301. doi: 10.1111/j.1600-051X.2006.00908.x.
3. Kim Y, Oh TJ, Misch CE, Wang HL. Occlusal considerations in implant therapy: clinical guidelines with biomechanical rationale. Clin Oral Implants Res. 2005;16(1):26-35. doi: 10.1111/j.1600-0501.2004.01067.x.
4. McAllister BS, Haghighat K. Bone augmentation techniques. J Periodontol. 2007;78(3):377-396. doi: 10.1902/jop.2007.060048.
5. Mercier P, Huang H, Cholewa J, Djokovic S. A comparative study of the efficacy and morbidity of five techniques for ridge augmentation of the mandible. J Oral Maxillofac Surg. 1992;50(3):210-217. doi: 10.1016/0278-2391(92)90314-P.
6. Sun HL, Huang C, Wu YR, Shi B. Failure rates of short (≤ 10 mm) dental implants and factors influencing their failure: a systematic review. Int J Oral Maxillofac Implants. 2011;26(4):816-825.
7. Atieh MA, Zadeh H, Stanford CM, Cooper LF. Survival of short dental implants for treatment of posterior partial edentulism: a systematic review. Int J Oral Maxillofac Implants. 2012;27(6):1323-1331.
8. Naenni N, Sahrmann P, Schmidlin PR, et al. Five-year survival of short single-tooth implants (6 mm): a randomized controlled clinical trial. J Dent Res. 2018;97(8):887-892. doi: 10.1177/0022034518758036.