Potential applications of exosomes in medicine and dentistry
Introduction
Exosomes are the smallest subset of extracellular vesicles that are nano-sized lipid bilayer particles secreted by nearly all cell types, serving as natural carriers of proteins, DNA, RNA, and mRNA that facilitate intercellular communication.1 Medical use of exosomes began more than 10 years ago and include improvements in tissue regeneration, neurogenesis, angiogenesis, and immune modulation.2 In dentistry, exosomes show immense promise for repairing many tissue types including dental pulp cells and periodontal tissues, all while mitigating inflammatory responses in conditions such as periodontitis.3
Despite their efficacy in preclinical models, substantial efforts are required to translate these findings into clinical practice. The ability of exosomes to alter their cargo in response to disease states further underlines their potential as a diagnostic and therapeutic tool in regenerative medicine.3
What are exosomes?
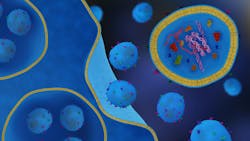
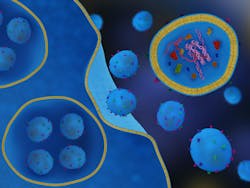
Exosomes are extracellular vesicles ranging in diameter from 30 nm to 150 nm that are secreted by virtually all cell types.4 They transport diverse biomolecules, including DNA, RNA, mRNA, and proteins for the benefit of either various cell types or tissues (figure 1). These endogenous particles contribute significantly to cellular efficacy and hold significant promise as diagnostic and therapeutic agents across various fields of medicine. The ability of exosomes to modulate cellular responses is at least partially attributed to their dynamic cargo profiles, thus offering new avenues for targeted cell delivery and improvements in disease treatment.3
The use of exosome-based strategies in medicine and dentistry is accelerated due to their high potential, including their effects on tissue regeneration in preclinical models conducted at various universities. They pose absolutely no threat to the immune system, which means there are no foreign body rejections that a patient needs to be concerned with unlike stem cell therapies.5
Role of exosomes in regenerative medicine
Exosomes have been extensively utilized as therapeutic agents to improve patient tissue regeneration. Among their remarkable abilities, they have been found to promote neural repair after injury while improving angiogenesis by forming new blood vessels. These processes are critical during tissue repair to ensure functional recovery of damaged systems. For example, exosomes derived from mesenchymal stem cells (MSCs) have been shown to facilitate cell differentiation and nerve tissue repair.2
Additionally, exosomes have been found to play a critical role in the regeneration of dental and periodontal tissues. Studies have demonstrated that exosome therapy is linked with the repair/regeneration of dental pulp tissues as well as periodontal structures damaged due to trauma or disease. Noteworthy, exosomes have played a key role in reducing inflammation in periodontal disease.3
Additionally, characteristics of exosomes include their ability to regulate immune responses and autoimmune disorders. By modulating both the innate and humoral immune systems, exosomes have been found to reduce inflammation and mitigate periodontally induced inflammation by altering cytokine production and immune cell activation.5 Exosomes that have been used specifically in the periodontal field are termed periosomes.
Preclinical research in animal models using periosomes has further highlighted the use of this specific subset of exosomes for precise disease treatment. Exosomes derived from these specific cell types have demonstrated the ability to modulate excessive immune responses without compromising the body’s ability to improve tissue regeneration.2
Applications in dentistry
Regeneration of dental pulp and periodontal tissues
Periosomes have gained particular attention in dentistry owing to their ability to improve tissue regeneration of dental pulp cells and periodontal tissues. These tiny vesicles encourage the proliferation and differentiation of dental tissues, aiding in their ability to repair various tissues. Their immunomodulatory properties further create a microenvironment conducive to healing.3
Reduction in periodontal disease activity
Periodontitis is characterized by the inflammation and destruction of supporting tooth structures and is one of the most prevalent diseases known to mankind. Noteworthy, periosome therapy has proven to be an effective and novel treatment option to reduce inflammation, promote tissue repair, and enhance the regeneration of alveolar bone and periodontal tissues. While preclinical models and results achieved in animal models are extremely positive, additional human clinical trials using periosomes are ongoing to further support these findings in humans for the benefit of our patients.5
Future directions
While exosomes hold great promise as a therapeutic tool, open questions are being addressed before their widespread application in clinical settings. A few limitations prior to universal use of exosomes include:
- Variability in exosome composition, depending on the cell of origin and conditions of release, their reproducibility as therapeutic agents remains a challenge.
- Detailed investigations are required into their long-term effects on the human body, particularly with engineered exosome products.
- Bridging the gap between preclinical findings and clinical applications will require additional studies focusing on dosage, delivery methods, and efficacy.
Despite these challenges, the potential of exosomes in both therapeutic and diagnostic realms represents enormous potential. Clinical investigators are now highly researching additional uses of exosomes over a wide spectrum of applications to provide better therapeutic outcomes in both medicine and dentistry.1
Conclusions
Exosomes are the future of regenerative medicine as well as dentistry and serve as pivotal tools to aid patients across a multiple of diseases. Their ability to heal patients by stimulating neurogenesis, promote angiogenesis, and regulate immune responses makes them invaluable options for regulating inflammation and speeding tissue repair. Particularly in dentistry, exosome-based therapies provide an innovative and promising approach for addressing current challenges that will help improve dental implant placement, treatment of periodontal disease, and endodontic treatments such as root canal therapy.
Nevertheless, exosome research is still in its infancy with respect to clinical applications. Much work remains to standardize their production, understand their mechanisms of action, and further support their increased safety and efficacy through clinical trials. Despite these hurdles, the future of exosome therapy is bright, offering hope for significant advancements in personalized medicine and dentistry.
Editor’s note: This article originally appeared in Perio-Implant Advisory, a chairside resource for dentists and hygienists that focuses on periodontal- and implant-related issues. Read more articles and subscribe to the newsletter.
References
- Miron RJ, Zhang Y. Understanding exosomes: part 1—characterization, quantification and isolation techniques. Periodontol 2000. 2024;94(1):231-256. doi:10.1111/prd.12520
- Miron RJ, Estrin NE, Sculean A, Zhang Y. Understanding exosomes: part 2—emerging leaders in regenerative medicine. Periodontol 2000. 2024;94(1):257-414. doi:10.1111/prd.12561
- Miron RJ, Estrin NE, Sculean A, Zhang Y. Understanding exososmes: part 3—therapeutic + diagnostic potential in dentistry. Periodontol 2000. 2024;94(1):415-482. doi:10.1111/prd.12557
- Ghosh A, Davey M, Chute IC, et al. Rapid isolation of extracellular vesicles from cell culture and biological fluids using a synthetic peptide with specific affinity for heat shock proteins. PloS One. 2014;9(10):e110443. doi:10.1371/journal.pone.0110443
- Mohammed E, Khalil E, Sabry D. Effect of adipose-derived stem cells and their exo as adjunctive therapy to nonsurgical periodontal treatment: a histologic and histomorphometric study in rats. Biomolecules. 2018;8(4):167. doi:10.3390/biom8040167
About the Author

Scott Froum, DDS
Editorial Director
Scott Froum, DDS, a graduate of the State University of New York, Stony Brook School of Dental Medicine, is a periodontist in private practice at 1110 2nd Avenue, Suite 305, New York City, New York. He is the editorial director of Perio-Implant Advisory and serves on the editorial advisory board of Dental Economics. Dr. Froum, a diplomate of both the American Academy of Periodontology and the American Academy of Osseointegration, is in the fellowship program at the American Academy of Anti-aging Medicine, and is a volunteer professor in the postgraduate periodontal program at SUNY Stony Brook School of Dental Medicine. He is a trained naturopath and is the scientific director of Meraki Integrative Functional Wellness Center. Contact him through his website at drscottfroum.com or (212) 751-8530.

Nathan Estrin, DMD
Nathan Estrin, DMD, received his bachelor’s degree in kinesiology from Indiana University and went on to earn his DMD from LECOM School of Dental Medicine. He received his training in periodontics at Stony Brook University in New York. During his dental studies, he developed a passion for regenerative, implant, and laser surgery and has more than 15 publications and three book chapters in these areas. Dr. Estrin is a board-certified periodontist in full-time private practice in Sarasota, Florida. He is also adjunctive faculty at LECOM School of Dental Medicine and a lead educator for PRFedu, where he trains dental offices on platelet-rich fibrin, lasers, and modern periodontal therapy.

Richard Miron, DDS
Richard Miron, DDS, is currently lead educator and researcher at Advanced PRF Education and an adjunct visiting faculty in the department of periodontology at the University of Bern, Switzerland, where he completed his PhD studies since 2009. Dr. Miron is a prolific author and international lecturer on topics relating to growth factors, bone biomaterials, and guided bone regeneration. He is widely considered one of the top contributors to implant dentistry. He has written 10 textbooks on regenerative dentistry including Next Generation Biomaterials for Bone and Periodontal Regeneration, Understanding Platelet Rich Fibrin, and Modern Implant Dentistry.