Patients with type 2 diabetes and tooth loss, gum problems more likely to be nutrient-deficient
A new joint, cross-sectional study by the Clinic Masae Minami/Minami Diabetes Clinical Research Center and the international oral health-care company Sunstar investigated the relationship between the number of teeth, self-reported gum condition, and intake of food and nutrition.
The study demonstrated that individuals with type 2 diabetes are more likely to lack key nutrients (such as dietary fiber, vitamins, and minerals) due to a decrease in the number of teeth and deterioration of the condition of their gums. These results underscore the importance of patients with type 2 diabetes receiving dietary advice specific to their oral health condition.
From Scott Froum, DDS, editorial director of Perio-Implant Advisory:
Tooth loss is a marker like anything else—e.g., inflammatory markers, A1c, and insulin resistance. The fact that tooth loss is correlated with nutrition, specifically fiber intake, is not surprising. When people eat processed foods or are nutritionally depleted, bad metabolic things happen—such as type 2 diabetes and a whole host of other issues like cardio, endocrine, and oral problems.
The real point is that when you have a patient with tooth loss and periodontal problems, you should be checking metabolic stability. That’s why I’m a PhD candidate in functional and integrative nutrition and am opening a clinic next to my dental office.
Researchers looked at oral health factors using a brief questionnaire, as well as physical indicators, including HbA1c and BMI. The study confirms there is a strong relationship between oral health and nutrient and food intake in patients with type 2 diabetes. Individuals with fewer teeth were shown to have lower consumption of plant protein and carotenes and were older. Poor gum condition was associated with lower intake of B vitamins (vitamin B1, vitamin B2, vitamin B6, folic acid, and pantothenic acid), vitamin C, total dietary fiber, and soluble and insoluble dietary fiber.
More about oral-systemic health ... Sugar consumption: Damaging more than just teeth
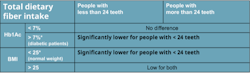
Study results also showed a significant correlation between the number of teeth and dietary fiber intake, after adjustment for age and sex—particularly for those with HbA1c levels of 7% or higher, where patients with fewer teeth showed lower dietary fiber intake. A similar relationship was observed in individuals with a BMI less than 25, while those with a BMI 25 or higher had consistently low dietary fiber intake regardless of the number of teeth.
While the results of this study alone do not reveal a causal relationship, it is expected that the quality of life for people with diabetes will be improved by receiving dietary advice according to their oral health condition, supporting them in chewing and eating.
Study methodology
The cross-sectional study involved 104 patients with type 2 diabetes who had 15 or more natural teeth, attending clinics. Indicators related to oral health (number of teeth and self-reported condition of gums ranging from very good to poor) were considered. A brief self-administered dietary history questionnaire was used to calculate crude daily intake to investigate food and nutrients. Physical indicators included HbA1c and BMI.
More about oral-systemic health ... Probiotic overuse and misuse: How to determine what probiotic your dental patient needs
Key research results
There is a relationship between number of teeth and condition of gums to intake of food and nutrients (Spearman’s ρ).
- Lower intake of green leafy vegetables, carrots/squash, as well as vegetable proteins and carotene were correlated with fewer teeth.
- People with self-reported poor gum health consumed less fish with bones, carrots/squash, and alcoholic beverages, as well as vegetable proteins, minerals including potassium, calcium,magnesium, carotenes, B vitamins, vitamin C, and soluble, insoluble, and total dietary fiber.
There is a relationship between the number of teeth and dietary fiber intake considering other factors (generalized linear model).
- When analyzing the intake of dietary fiber (considered crucial in dietary therapy for diabetic patients), a significant correlation was shown between more teeth and a greater intake of total dietary fiber, adjusting for gender and age.
- Subjects were clustered based on their metabolic control (HbA1c) and number of teeth and compared to total dietary fiber intake, again adjusting for gender and age. In the group with an HbA1c less than 7%, there was no association between the amount of total dietary fiber and number of teeth. However, in the group with poor metabolic control (HbA1c ≥ 7%), total daily dietary fiber intake was significantly lower in the group with substantial tooth loss (having fewer than 24 teeth), compared to the group having 24 or more teeth (figure 1: upper row).
- Study subjects were also clustered according to their BMI. Surprisingly, in the group with a BMI lower than 25 (considered healthy), it was shown that total dietary fiber intake was significantly lower in those with substantial tooth loss (having fewer than 24 teeth), compared to those with 24 or more teeth. In patients with a BMI ≥ 25 (considered obese), the values were low in both groups, and there was no difference between the groups (figure 1: lower row).
Research background and purpose
It is often reported that the decrease in number of teeth affects the amount and diversity of food intake and nutrients. Patients with type 2 diabetes have a high risk of developing periodontal disease and are prone to tooth loss, and there is concern that a subsequent decline in oral function could make appropriate dietary therapy difficult. However, the relationship between oral health and nutrition and food intake in diabetic patients is not well understood.
This study aimed to clarify the relationship between oral health and nutrient and food intake in patients with type 2 diabetes and is part of Sunstar’s efforts to promote research about the connection between oral and general health. For more than 30 years, the company has been raising awareness about the connection between oral health and systemic diseases (particularly diabetes), driven by the personal story of the company’s founder, Kunio Kaneda. Kaneda suffered from diabetes and eventually lost his battle with it at a relatively young age. Since then, Sunstar has focused on the relationship between diabetes and periodontal disease and is engaged in ongoing research, new product development, and awareness in collaboration with universities and medical institutions.
Note: The results of this study were presented at the 66th Annual Meeting of the Japan Diabetes Society in May 2023.
Source: This content is based on a press release dated November 8, 2023, from Sunstar.