Are you screening for sleep apnea when treatment planning occlusal guards?
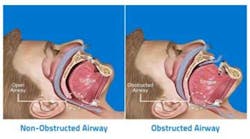
When treatment planning for bruxism, many clinicians have been trained only to observe the 3 T’s: teeth, trauma, and TMJ. In some instances, treatment planning an occlusal guard when noting clenching or grinding may be a misdiagnosis. Bruxism, in some cases, can be a result of sleep apnea, as opposed to a symptom of TMD. In patients with OSA, teeth grinding can occur as a reactionary mechanism to wake the body during sleep when there is a lack of proper oxygen intake. A percentage of patients, including children, actually grind their teeth to wake themselves when the body is gasping for air during moments of apnea. Their bruxism may be a direct result of untreated sleep apnea.
ADDITIONAL READING |Hidden dental dangers of undiagnosed obstructive sleep apnea
If patients feature some of the anatomical associations with OSA in addition to bruxism, then treating them with an occlusal guard may be the incorrect treatment modality. It is important to have patients at risk for OSA fill out an Epworth Sleepiness Scale form. A determination of their overall fatigue, energy level, snoring frequency, and daytime sleepiness can be assessed with the Epworth Sleepiness Scale. Following this assessment, if patients are at risk for having OSA, a polysomnograph (PSG) with a sleep technician should be scheduled. Only a physician such a pulmonologist or an ENT can actually diagnose obstructive sleep apnea from the results of the PSG. If a determination is made from the physician that the patient’s OSA can be alleviated with treatment other than CPAP, a custom-fitted oral appliance, such as a mandibular-positioning or a tongue-retaining device, could be considered for treatment with the proper assessment.
Dental professionals need to become properly trained in the field of sleep medicine to be more well versed with OSA. Understanding the physical manifestations that present with OSA in the oral cavity is imperative. In addition, becoming knowledgeable about the different types of oral appliances to treat OSA with or without CPAP is also necessary. Bruxism can be a byproduct of OSA, and some PSGs actually account for the number of bruxism episodes during a sleep cycle. Treatment planning an occlusal guard to treat the bruxism that is a result of OSA is not addressing the source of the pathology. If left untreated, sleep apnea can lead to significant health problems in patients. Some of the health risks associated with sleep apnea include type 2 diabetes and serious cardiovascular health ailments such as heart disease, stroke, heart attacks, and heart failure. It is estimated that 22 million Americans suffer from sleep apnea, and this statistic will only continue to rise with a growing population. Dentists must play their part in helping screen patients correctly for OSA. If patients present with bruxism, an occlusal guard may not be the only treatment solution. So, the next time you ask your patients if they grind their teeth, also ask them if they snore.