The American Academy of Periodontology warns of a significant public health problem: One out of every two American adults 30 years and older has periodontal disease. (1) As dental professionals, we need to step up to this challenge and change the way we evaluate and treat mucosal oral infections. The research, tools, and biologic products are now available to regenerate bone and tissue—not simply “manage or repair”!
Today, more than 90% of patients with periodontal disease are treated with scaling/root planing (SRP) and/or antibiotics only. The other 7% to 9% are offered surgical treatments, and only 1% to 3% of patients are ever offered a regeneration procedure. (2,3)
ADDITIONAL READING |Does your dental extraction socket need a bone graft: A decision matrix
Dental professionals hold the key role to identifying periodontal infections in the oral cavity that act as a reservoir for proinflammatory mediators that enhance the inflammatory response to induce a systemic effect that can affect the overall health of the patient.
The goal of true periodontal regenerative therapy for periodontal disease is the restoration of the lost form and function of the peridontium with new cementum, a functionally oriented periodontal ligament, and most importantly, formation of new alveolar bone.
ADDITIONAL READING |Guided tissue regeneration: background to current indications and applications
Traditional periodontal treatment utilizing only SRP with or without antimicrobial therapy often results in only repair of the periodontium. Periodontal repair implies healing with connective tissue and/or long junctional epithelium that does not fully restore architecture and form (i.e., scar tissue). Regeneration is the body’s reproduction of lost tissue and/or bone to its original form and that should be the goal of treatment.
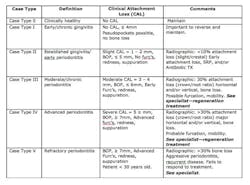
Our role as dental professionals is to identify the optimal time for regenerative periodontal therapy. Periodontal disease patients with moderate to advanced Case Type III or higher are candidates for periodontal regenerative therapy, according to the 2014 new case types for periodontal disease by the Academy of Periodontology, outlined by Dr. G. Armitage (see Table 1). (4) Note the comment section on when to refer for regenerative treatment for the best, long-lasting results for the patient’s overall health.
To achieve predictable periodontal therapy results, a guided bone/tissue regeneration procedure (GTR/GBR) is indicated that includes the use of bone-grafting products (e.g., enamel matrix derivative) to regenerate the lost tissue and, most importantly, the bone. (5-8)
Regeneration dentistry involves new protocols and standards of care: doctors evaluating for soft tissue and bone loss in exams, hygienists providing accurate data, identification of areas of concern, and the entire dental team discussing the new treatment options available. Are you ready to take the challenge? Think regeneration—not manage or repair!
References
1. WHO Global Oral Health Program/http://www.dent.niigata-u.ac.jp/prevent/perio/perio.html.
2. AAP position paper: Epidemiology of periodontal diseases. J Periodontol 2005;76:1406-1419.
3. Loesche WJ, Grossman NS. Periodontal disease as a specific, albeit chronic, infection: Diagnosis and treatment. Clin Microbiol Rev 2001;14:727-752.
4. Armitage GC. Commentary: Evolution and application of classification systems for periodontal diseases—a retrospective commentary. J of Periodontol 2014;85(3):369-371.
5. Lemmerman KJ, Lemmerman NE. Osseointegrated dental implants in private practice; a long-term case series study. J Periodontol. 2005;76(2):310-319.
6. Attard NJ, Zarb GA. Long-term treatment outcomes in edentulous patients with implant-fixed prostheses: the Toronto study. Int J Prosthodont. 2004;17(4):425-433.
7. Lambrecht JT, Filippi A, Kunzel AR, Schiel
HJ. Long-term evaluation of submerged and nonsubmerged ITI solid-screw titanium implants; a 10-year life table analysis of 468 implants. Int J Oral Maxillofac Implants. 2003;18(6):826-834.
8. Wingrove S. Peri-Implant Therapy for the Dental Hygienist: A Clinical Guide to Implant Maintenance and Disease Complications. John Wiley and Sons, 2013.