Treating young patients with ectodermal dysplasia: A prosthetic dilemma
Prosthodontist Kim Daxon, DDS, is used to treating children and adolescents who desperately need the expertise of a multidisciplinary specialist team for their dental care. Her new patient—a referral from a local pediatric dentist—is nine years old and has ectodermal dysplasia. Follow along to see how Dr. Daxon approaches the challenge of treatment planning for this multifaceted case.
Memories of toy trunks, cartoon stickers, and bitter fluoride trays typically come to mind when the topic of pediatric dentistry arises. Today, as a practicing prosthodontist, I rarely see children who need routine dental care, where stickers fall a little short of a reward for good behavior. Much more often, I see children and adolescents who desperately need the expertise of a multidisciplinary specialist team for their dental care.One in every 10,000 children are affected with ECTODERMAL DYSPLASIA (ED), A HEREDITARY CONDITION IN WHICH TWO OR MORE ECTODERMAL STRUCTURES UNDERGO ALTERATIONS IN DEVELOPMENT OR DO NOT DEVELOP AT ALL. (1–2)
The challenges we face as dental professionals
Children afflicted with ED will have an abnormal appearance, and they often suffer from low self-esteem. They tend to have thin, light-colored, sparse hair; smooth, dry, and thin skin; and missing teeth. The most distinguishing oral characteristics include hypodontia or anodontia, hypoplastic conical teeth, and underdevelopment of the alveolar ridges. (3) These patients may also suffer from malocclusion, periodontal damage, reduced chewing ability, nutritional deficiencies, and speech problems. (4) Those complications can make decisions on treatment especially difficult.
The developmental challenges with ED lead to complicated and expensive prosthetic treatment lasting several years. Prosthodontic treatment goals are aimed at creating a normal dental appearance so the patient’s physiologic and psychosocial well-being are preserved.
AJ Nowak stated in the Birth Defects Research Journal: “Treating the pediatric patient with ED requires the clinician to be knowledgeable in growth and development, behavioral management, techniques in the fabrication of a prosthesis, the modifications of existing teeth utilizing composite resins, the ability to motivate the patient and parent in the use of the prosthesis, and the long-term follow-up for the modification and/or replacement of the prosthesis.” (5)
A nine-year-old female was referred to me by a local pediatric dentist (figure 1). The pediatric dentist felt she had reached the limit in what she could provide for the patient cosmetically. The patient had received only routine dental care and cosmetic bonding thus far. She was entering fourth grade in school and was becoming increasingly self-conscious about her smile (figure 2).
Examination and medical diagnosis
Upon clinical and radiographic examination, the patient presented with multiple missing permanent teeth (figures 3, 4a, and 4b). Tooth No. 8 was malpositioned and slightly mobile. Her mandibular dentition was stable and intact, although mostly deciduous (figure 5). Upon further questioning, I learned that her brother had a similar condition. Taking into consideration the patient’s physical appearance and the genetic similarity to her brother, I discussed with her parents the need to obtain a medical diagnosis through genetic testing.
I learned from my mentor and friend, Dr. Bob Faulkner, that obtaining a medical diagnosis for patients with these types of issues is crucial. I knew that her dental rehabilitation was going to be long and expensive, and the medical diagnosis would be necessary for medical insurance to provide the financial resources (figure 6).
Figure 6
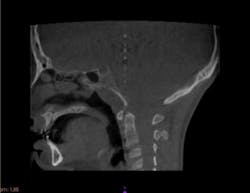
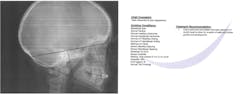
I also recommended that the patient see an oral surgeon for a baseline cone beam computed tomography (CBCT) as well as an orthodontist for a baseline cephalometric analysis (figures 7 and 8). It is important to evaluate the existing skeletal structures and monitor growth over time, so decisions can be made regarding appropriate treatment options and the timing of treatment.
Figure 7
Figure 8
Treatment options: The how, why, and when
In addition to restorative dentistry, other treatment options such as fixed, removable, and implant prosthodontics are available. (6) Fixed partial dentures (FPDs) are rarely used, because many patients with ED are missing so many teeth, retention form is poor on the conical crowns, and pulp chambers are large. Also, FPDs are generally contraindicated if the patient is actively growing, because they can negatively affect jaw growth, especially if the prosthesis crosses the midline. (7) Removable partial dentures, complete dentures, and overdentures are the most common methods used to treat patients afflicted with ED. These prostheses must be monitored every six to 12 months for fit and occlusal changes as growth occurs, and then remade when necessary. Other challenges with removable prostheses are dietary limitations, speech difficulties, and loss of the prosthesis. (5)
Generally, placing implants in a patient who is still growing is considered to be against industry-wide standards for care; however, placing implants in young patients with ED should be considered. Determinations will need to be made about the cessation of skeletal growth to ensure it’s safe to place implants in these young adults. Several unfavorable potential effects—including trauma to tooth germs, tooth eruption disorders, and multidimensional restrictions of skeletal growth—can prevent placing implants and lead to unacceptable esthetic outcomes. (8)
Placing implants in a child with ED can have a significant effect on his or her social and psychological well-being (9) The possibility of preserving the alveolar bone is another reason to consider placing implants. (10) Due to a lack of tooth development, the alveolar ridges in these patients are underdeveloped and must support a dental prosthesis over the course of their lifetime. If possible, it is recommended to delay implant placement at least until the age of 13 when alveolar growth has slowed down (11).
The prosthetic dilemma
Understanding and knowing the best treatment plan and treatment timing for this patient is difficult and depends upon the answers to the following questions:
- What is the psychological/emotional status of the patient with respect to how she feels about the way she looks?
- What are the functional and phonetic limitations?
- Are there significant nutritional and dietary concerns as a result of missing so many teeth?
- Should deciduous teeth be maintained for as long as possible to “preserve bone?”
- If implants are needed to support a prosthesis, is there adequate interarch space?
- How do we manage the patient prosthetically, and how often do the prostheses need to be replaced as continued growth occurs?
- Are there psychological benefits to having fixed over removable?
- What are the estimated costs of treatment over time?
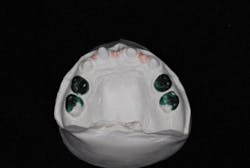
Before a treatment plan can be developed, it is crucial to make an accurate dental diagnosis. Although the patient was only nine years old, it was necessary to outline diagnostic protocols to thoroughly evaluate and diagnose. We started with a complete exam, diagnostic photographs, and study casts mounted in centric relation (figures 9a and 9b). Through these records, we were able to determine the patient’s ideal tooth position to satisfy her esthetic goals. We discussed treatment options on how to achieve these results with both the patient and the parents (figure 10).
Figure 10
Conclusion
Managing young patients with ectodermal dysplasia is prosthetically challenging and creates many treatment decision dilemmas. Ultimately, the decision to begin treatment in patients with ED should be made by the treating dentist, the parents, and the patient. My training at The Dawson Academy provided me with a systematic checklist and protocol for making a complete diagnosis, which led to an acceptable treatment plan and, ultimately, a very happy patient.
Editor's note: This article was contributed by The Dawson Academy.
References
1. Cezária Triches T, Ximenes M, Oliveira de Souza JG, Rodrigues Lopes Pereira Neto A, Cardoso AC, Bolan M. Implant-supported oral rehabilitation in child with Ectodermal dysplasia—4-year follow-up. Bull Tokyo Dent Coll. 2017;58(1):49-56. doi: 10.2209/tdcpublication.2016-0012.
2. Shah KN. Ectodermal dysplasia. Medscape website. https://emedicine.medscape.com/article/1110595-overview. Published February 24, 2016. Accessed December 11, 2017.
3. Levin LS. Dental and oral abnormalities in selected ectodermal dysplasia syndromes. Birth Defects Orig Artic Ser. 1988;24(2):205-227. PMID:3052618.
4. Clauss F, Manière MC, Obry F, et al. Dento-craniofacial phenotypes and underlying molecular mechanisms in hypohidriotic ectodermal dysplasia (HED): a review. J Dent Res. 2008;87(12):1089-1999.
5. Nowak AJ. Dental treatment for patients with ectodermal dysplasias. Birth Defects Orig Artic Ser. 1988;24(2):243-252.
6. Pigno MA, Blackman RB, Cronin RJ Jr, Cavazos E. Prosthodontic management of ectodermal dysplasia: a review of the literature. J Prosthet Dent. 1996;76(5):541-545.
7. Hogeboom FE. Restorative procedures for children with ectodermal dysplasia. ASDC J Dent Child. 1961;28:62-72.
8. Kramer F-J, Baethge C, Tschernitschek H. Implants in children with ectodermal dysplasia: a case report and literature review. Clin Oral Impl Res. 2007;140-146. doi: 10.1111/j.1600-0501.2006.01180.x.
9. Kent G. Effects of osseointegrated implants on psychological and social well-being: a literature review. J Prosthet Dent. 1992;68(3):515-518. doi: 10.1016/0022-3913(92)90421-6.
10. Murphy VM. Clinical and experimental bone changes after intraosseous implantation. J Prosthet Dent. 1995;73(1):31-15.
11. Guckes AD, Brahim JS, McCarthy GR, Rudy SF, Cooper LF. Using endosseous dental implants for patients with ectodermal dysplasia. J Am Dent Assoc. 1991;122(10):59-62.