Patient dose reduction in dental imaging
By Gail F. Williamson, RDH, MSIntroduction Dental radiographic examinations and their associated risks have been a topic of discussion in the national media recently. The Dr. Oz television show, CNN.com, and The New York Times all have featured discussions or articles regarding the necessity or frequency of dental radiographs and associated risks. Although the cancer risk from dental radiographic examinations is thought to be negligible, no radiation exposure is risk-free and the effects of radiation are cumulative. Dental professionals have an ethical obligation to comply with the ALARA principle and keep the radiation dose to the patient As Low As Reasonably Achievable. There are many ways that this can be accomplished, and these measures will be discussed in the subsequent text. Risk assessment Dental radiographic examinations are invaluable tools necessary for the diagnosis and treatment of oral diseases. The primary risk from dental radiography is radiation-induced cancer. The risk of cancer as a result of low-dose radiation is difficult to estimate. Risks have been estimated by extrapolation of high radiation dose data from Japanese atomic bomb survivors and other exposed populations. The reported average effective dose for an intraoral or a panoramic radiographic examination is much smaller than the minimum dose for which risk can be determined.1,2 The Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation (BEIR VII) concluded that the preponderance of evidence indicates that there is some risk at low doses but the risk is small.3 The National Council on Radiation Protection (NCRP) Report 145 concluded that radiation risks to dental patients and operators are very small and may be zero.2 In 2007, the International Council on Radiation Protection (ICRP) updated the method for calculating effective dose based on the latest scientific information on the biology and physics of radiation exposure.4 The effective dose is used to estimate risk or assess biologic consequences in human beings. It is the sum of weighted equivalent doses for the radiosensitive tissues of the body. An investigation by Ludlow et al. applied the 2007 ICRP tissue-weighting factors and calculation method to typical dental radiographic examinations.5 The results indicate that the effective doses for various intraoral and extraoral radiographic examinations were 32% to 422% higher than those calculated according to previous ICRP guidelines. The investigators concluded that the increases in the effective doses of common radiographic examinations were high enough to warrant reconsideration of methods to reduce patient exposure.5 Other investigations have suggested a possible association between exposure of the thyroid gland during pregnancy and low birth weight infants and an increased risk of thyroid cancer both as a result of dental radiographic examinations.6,7 These publications and others have prompted renewed interest in the risks of dental radiographic examinations and the importance of patient radiation safety and protection measures.Patient concerns First and foremost, dental professionals must take the radiation concerns of dental patients seriously. Patients become alarmed when they see and hear news reports about the dangers of radiation exposure and cancer. It is important to take time to discuss their concerns and effectively communicate why radiographs are necessary when indicated, what the benefits of the examination are relative to diagnosis and treatment, and what measures will be taken to keep the exposure as low as possible. Justification of the radiographic examination and determination that the benefit outweighs the risk are fundamental concepts in prescribing radiographs. All too often, dental radiographs are taken at fixed intervals without any explanation or consideration of the patient’s oral condition, medical/dental history, frequency of dental care, and other factors that could inform the practitioner of the need and frequency of a radiographic examination. Dental patients are left with the impression that the prescription for dental radiographs is not evidenced-based but rather arbitrary and unnecessary. Not all patients require the same radiographic examination nor at the same frequency. “One size does not fit all.” The purpose of selection criteria guidelines is to assist dentists in making appropriate prescriptions for dental radiographs.Guidelines for dental radiographic examinations Guidelines for prescribing dental radiographs have been available for nearly 25 years. In 2004, the American Dental Association (ADA) and the U.S. Food and Drug Administration (FDA) updated the original document to better reflect current practice.8 The use of selection criteria is the recommended method for identifying patients who will benefit from a radiographic examination. The guidelines follow these basic concepts: type of encounter (new or recall), patient age (child, adolescent, adult), stage of dental development (primary, transitional, permanent dentitions; partially edentulous, edentulous), vulnerability to known risk factors (caries, periodontal disease) growth and development monitoring, and other circumstances.8 The overarching theme is that the dentist should discuss the medical and dental history with the patient, perform a clinical examination to look for signs or symptoms of disease, and determine necessary radiographs based on the information gathered and the expectation that the radiographs will provide evidence that will affect diagnosis and treatment planning. The use of selection criteria guidelines is a primary concept in reducing patient radiation exposure. Patient examinations should be individualized and only necessary, high-yield radiographs should be taken rather than unjustified routine radiographs. Routine, fixed schedules for radiographic examinations for all patients are not recommended except as outlined in the bitewing guidelines according to caries risk. Once the decision to obtain radiographs is made, the practitioner should attend to the ALARA principle and use best practices with regard to receptor selection, X-ray beam collimation, exposure and processing techniques, and patient shielding.8 Since radiographs are typically delegated, staff members must have the necessary credentials and requisite skills to ensure that diagnostic images are produced with minimal or no retakes. Steps to reduce dental patient radiation exposure The ADA Council on Scientific Affairs, the NCRP, and American Academy of Oral and Maxillofacial Radiology (AAOMR) have published reports that provide guidance on methods to reduce radiation exposure to dental patients.2,9,10 All of these documents endorse the use of selection criteria and other measures to reduce patient exposure. The measures that most significantly impact dose reduction include the use of selection criteria, fast film or digital receptors for intraoral radiography, rare earth screen-film combinations or digital receptors for extraoral radiography, and rectangular collimation of the X-ray beam.11Intraoral receptors (Fig. 1) The use of faster intraoral receptors can significantly decrease the exposure to the patient. Use of F-speed film reduces exposure 25% compared to E and 60% compared to D-speed film. The FDA recommends that film below E-speed not be used for dental radiography because it contributes to greater than necessary patient exposure.12
Fig. 1 — Available intraoral image receptors include film, phosphor plate, and rigid sensors. Digital receptors are available in two basic formats, photostimulable phosphor plates (PSP) and wired or wireless rigid sensors including the charge-coupled device (CCD) and the complementary metal oxide semi-conductor (CMOS). Phosphor plate receptors most closely approximate film in terms of size, thickness, and handling. The greatest disadvantages of phosphor plate receptors are emulsion abrasion that may necessitate plate replacement and the scanning step which delays image viewing. By contrast, wired or wireless rigid digital receptors are thicker and more rigid in their construction. The primary disadvantages of rigid receptors are the smaller active image area, which may increase the number of images taken, and rigidity, which can cause discomfort. Rigid digital receptors are more difficult to use initially and produce more technical errors when compared to film and plate receptors.13-15 The estimated exposure reduction for digital receptors ranges from 30% to 60% with the mean reduction of 55%.13,16 The actual amount of exposure reduction achieved with digital receptors is dependent on a number of factors including speed, receptor performance, technique, and retakes. Results of a systematic review of digital intraoral radiography suggest that a dose reduction may not be realized due to a greater number of images taken, patient discomfort, errors, and retakes.16Extraoral receptors High-speed rare earth screen-film combinations can reduce exposure by 55% for panoramic and cephalometric radiographs.17 Digital receptors can be used for extraoral radiography as well. Photostimulable phosphor plates are available in panoramic and cephalometric sizes and can be placed inside the film cassette. CCD or CMOS digital panoramic and cephalometric systems are also available. There is no significant dose reduction achieved with using digital receptors instead of rare-earth intensifying screens combined with matched high-speed film for extraoral radiography.17Rectangular collimation Rectangular collimation restricts the size of the X-ray beam, exposes 70% less tissue volume than round collimation, and decreases the effective dose to the patient approximately fivefold.18,19 Additionally, rectangular collimation reduces scatter radiation and improves image geometry. Other devices that provide rectangular collimation include rectangular collimators that attach to round PIDS, metal rings that clip into the instrument beam guide, or facial shield collimators incorporated into receptor-holding instruments. (Fig. 2) The use of longer open-ended source-to-object devices (16” or 40 cm) rather than short (8” or 20 cm) are recommended.2 Increased distance results in approximately a 30% reduction in exposed tissue volume and a further reduction in thyroid exposure.17 (Fig. 3)
Fig. 2 — Rectangular collimation can be achieved with a rectangular PID, an attachable device for round PIDs, metal rings that clip into the instrument beam guide or facial shield collimators incorporated into the receptor-holding instrument.
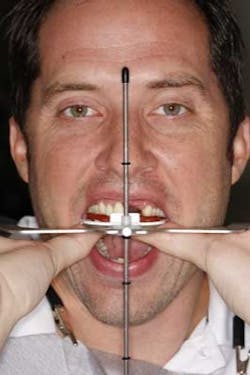
Fig. 3 — Longer PIDs that achieve a greater source-to-object distance can further reduce the volume of tissues exposed at the skin surface.Patient shielding The thyroid gland, particularly in children, is among the most sensitive organs to radiation-induced tumors.2 The use of a thyroid collar results in a 50% or greater exposure reduction to the gland.20 The NCRP recommends use of the thyroid collar for children and adults when it does not interfere with the image study, and the ADA recommends that a thyroid collar should be used on all patients for intraoral radiography, especially children and pregnant women.2,8 (Fig. 4) The selection criteria guidelines recommend that a protective thyroid collar and lead apron be used whenever possible and strongly recommends their use when imaging children, women of childbearing age, and pregnant women.2 The NCRP indicates that a lead apron need not be provided if all other recommendations in the report are followed rigorously.2 NCRP report 145 includes more than 100 recommendations that require compliance in order to dispense with lap apron shielding.2,11
Fig. 4 — Thyroid collars significantly reduce exposure to the gland and are particularly important when imaging children and pregnant women.
Beyond those previously discussed, there are additional measures — which are detailed in the NCRP, ADA, AAOMR publications2,8,9,10 — that can be employed to further reduce dose and attend to the ALARA principle.Summary Dental radiographic examinations are not without risk. The biologic effects of radiation are cumulative and every effort must be taken to keep radiation exposures as low as reasonably achievable. A variety of radiation safety and protection measures can be employed to reduce exposure to dental patients. Chief among these are selection criteria, receptor selection, rectangular collimation, and patient shielding.
Beyond those previously discussed, there are additional measures — which are detailed in the NCRP, ADA, AAOMR publications2,8,9,10 — that can be employed to further reduce dose and attend to the ALARA principle.Summary Dental radiographic examinations are not without risk. The biologic effects of radiation are cumulative and every effort must be taken to keep radiation exposures as low as reasonably achievable. A variety of radiation safety and protection measures can be employed to reduce exposure to dental patients. Chief among these are selection criteria, receptor selection, rectangular collimation, and patient shielding.
Gail F. Williamson is a professor of dental diagnostic sciences in the Department of Oral Pathology, Medicine and Radiology at Indiana University School of Dentistry in Indianapolis, Ind. She serves as director of Allied Dental Radiology and course director for dental assisting and dental hygiene radiology courses. Prof. Williamson is a published author and presents nationally on topics in oral and maxillofacial radiology.References 1. United Nations Scientific Committee on the Effects of Atomic Radiation. Sources and the Effects of Ionizing Radiation. Volume 1, Sources, UNSCEAR 2000 Report to the General Assembly, with References. Publication E.00.IX.3. United Nations, New York. 2. National Council on Radiation Protection and Measurements. Radiation protection in dentistry. NCRP Report No. 145. Bethesda, MD. National Council on Radiation Protection and Measurements, 2003. 3. National Academy of Sciences/National Research Council. Health effects of exposure to low levels of ionizing radiation. Committee on the Biological Effects of Ionizing Radiation (BEIR VII Phase 2). Washington: National Academy Press, 2006. Available at: http://books.nap.edu/catalog/11340.html Accessed Oct. 7, 2011. 4. Valentin J. The 2007 Recommendations of the International Commission on Radiological Protection. Oxford, England: Elsevier; 2007. 5. Ludlow JB, Ludlow LE, White SC. Patient risks related to common dental radiographic examinations: the impact of 2007 International Commission on Radiological Protection recommendations regarding dose calculations. JADA 2008; 139:1237-1243. 6. Hujoel P, Bollen A-M, Noonan CJ, del Aguila MA. Antepartum dental radiography and infant low birth weight. JAMA 2004; 291:1187-1193. 7. Memon A, Godward S, Williams D, Siddique I, Al-Saleh K. Dental X-rays and the risks of thyroid cancer: A case-controlled study. Acata Oncologica, 2010; 49:447-453. 8. U.S. Department of Health and Human Services, Public Health Service, Food and Drug Administration and American Dental Association, Council on Dental Benefit Programs, Council of Dental Practice, Council on Scientific Affairs. The selection of patients for radiographic examinations. Rev. Ed. 2004. Available at: http://www.ada.org/2760.aspx?currentTab+2 Accessed Oct., 11, 2011. 9. American Dental Association Council on Scientific Affairs. The use of dental radiographs: update and recommendations. JADA 2006; 137:1304-1312. 10. White SC, Heslop EW, Hollender LG, Mosier KM, Ruprecht A, Shrout MK. Parameters of radiologic care. An official report of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2001; 91:498-511. 11. Preece J. NCRP radiation protection in dentistry — a challenge for the dental profession. AADMRT Newsletter, Winter 2011. Available at: http://www.aadmrt.com/static.aspx?content=currents/ptreece_winter_11 Accessed Sept. 30, 2011. 12. U.S. Food and Drug Administration Center for Devices and Radiological Health. Dental radiography: Doses and film speed. Available at: http://www.fda.gov/Radiation-EmittingProducts/RadiationSafety/NationwideEvaluationofX-RayTrendsNEXT/ucm116524.htm Accessed Oct. 18, 2011. 13. Wenzel A, Moystad A. Experience of Norwegian general dental practitioners with solid state and storage phosphor detectors. Dentomaxillofac Radiol 2001; 30:203-208. 14. Sommers TM, Mauriello SM, Ludlow JB, Platin E, Tyndall DA. Preclinical performance comparing film and CCD-based systems. J Dent Hyg 2002; 76:26-33. 15. Bahrami G, Hagstrom C, Wenzel A. Bitewing examination with four digital receptors. Dentomaxillofac Radiol 2003; 32:317-321. 16. Wenzel A, Moystad A. Work flow with digital intraoral radiography: A systematic review. Acata Oncologica Scandinavica, 2010; 68:106-114. 17. Pharoah MJ, White SC. Oral Radiology: Principles and Interpretation, 6th Ed. St. Louis: Mosby Inc., 2009:37. 18. Gijhels F, Jacobs R, Sanderink G, De Smet E, Nowak B, Van Dam J et al. A comparison of the effective dose from scanography with periapical radiography. Dentomaxillofac Radiol 2002; 31:159-163. 19. Gibbs SJ. Effective dose equivalent and effective dose: Comparison for common projections in oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90:538-545. 20. Langland OE and Langlais RP: Principles of Dental Imaging, 2nd Ed., Philadelphia: Lippincott Williams & Wilkins, 2002:322.