A unique method of debriding a full-arch, maxillary prosthesis supported by dental implants
The role of endosseous dental implants in the restoration of patients has evolved dramatically since the original treatment concepts spearheaded by P.I. Branemark in the early 1970s. Treatment philosophies have expanded from the original concept that offered a fixed solution for patients who were rendered edentulous in the mandible to our being able to provide single-tooth replacement that closely mimics the hard- and soft-tissue esthetics of the original dental unit.
The original concept involved a cautious approach, whereby machined-surface implants were inserted with excellent primary stability in good quality bone through the use of a two-stage approach, and only uncovered and loaded after at least six months. The prostheses were designed to restore the implants using treatment pathways extrapolated from complete denture prosthetics, commonly involving the veneer of precious metal gold frameworks with acrylic resins. Prostheses were designed such that a considerable space was maintained between the fitting surface and the underlying soft tissues, and they always opposed maxillary, complete removable dentures.
ADDITIONAL READING |Restoration of a damaged dental implant due to removal of a fractured screw: thinking outside the box
These early protocols have been extrapolated over time such that fixed, full-arch, implant-supported prostheses are now being proposed as a treatment solution for the maxilla in addition to the mandible. Furthermore, advances in implant micro and macro geometry design and surface treatment technology have allowed for faster osseointegration. This has led to immediate implant insertion following tooth extraction and immediate prosthesis insertion as a treatment solution that is now commonplace.
ADDITIONAL READING |Interdisciplinary management of a complex maxillary implant restoration
However, technological and treatment advances are not without their problems. Metal-acrylic, hybrid prostheses—while they demonstrated adequate longevity when opposing complete dentures—suffer from accelerated wear when opposing a natural dentition or, worse, implant-supported prostheses. This is in addition to recurring problems associated with abutment and prosthetic screw loosening and fracture. Exposure of the underlying metal framework may eventually result in fracture of the entire prosthesis and, therefore, failure. (Figures 1 and 2)
Anatomical considerations specific to the maxilla often result in full-arch prostheses that have concave, tissue-fitting surfaces with extended flanges. These are usually essential, not only to provide adequate lip support, but also a seal to prevent the escape of air that would otherwise cause a whistling sound during speech. It is also not uncommon to find that the implant fixture heads are positioned too far coronally in relation to the optimal cervical margins of the teeth, such that the prosthetic teeth need to be set up with a degree of “ridge overlap.” These design implications often create prostheses that are impossible to debride both by the patient as well as the dental professional. The situation is further compromised by the fact that these prostheses are commonly provided to patients who have lost their natural dentition as a result of periodontal disease. (Figure 3) Statistically this puts them at a significantly higher risk of developing peri-implant disease.
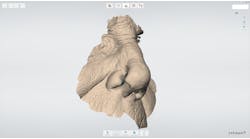
This high incidence of both technical and biological complications has led to our philosophy that providing all patients who have been restored with a fixed, full-arch prosthesis with a spare prosthesis is highly desirable. In most situations, the provisional prosthesis naturally transitions into the “spare” prosthesis once the definitive prosthesis has been fitted. However, advances in prosthesis manufacturing using CAD/CAM technology have made it relatively cost-effective to provide patients with spare, definitive prostheses. This offers the clinician a luxury of being able to rotate the prostheses on a two- to three-year basis so that they can be thoroughly and effectively debrided, disinfected, and refurbished where required. The elegance of this approach is that, with screw-retained prostheses, very little chairside time is required. (Figures 4-12) Rectifying problems and cleaning prostheses would historically take up considerable time, during which the patient had to remain in the dental office.
Conventional composite/acrylic-metal hybrid prostheses are best disinfected by immersion in various proprietary solutions for a reasonable time. Solutions can include 1% sodium hypochlorite, 2% glutaraldehyde, 2% chlorhexidine digluconate, or 3.8% sodium perborate. However, care must be taken to ensure that the chemical compositions of the solutions do not have an adverse effect on the surface properties of the metal frameworks as well as the mechanical and surface properties of the various veneering materials.
One alternative includes exposure to ultraviolet light or microwave radiation. Mechanical cleaning can be achieved manually with the advantage of excellent access once the prosthesis has been removed. Additional options include immersion in an ultrasonic bath or the use of pressurized steam cleaners.
Recently, we tested the use of vacuum autoclaves to actually sterilize as well as disinfect bonded porcelain restorations, being resistant to much higher temperatures, and we have experienced no adverse effects. This approach is not advisable for all-ceramic zirconia restorations, because accelerated hydrothermal aging of this compound occurs causing a decrease in flexural strength as a result of the transformation from tetragonal to monoclinic crystal structure.
The key factor that is essential to achieve successful disinfection with any of the above techniques is that a suitable exposure time to the disinfecting agent is required. Conventionally, this would directly occupy in-office time, but a spare prosthesis offers a much more cost-effective and time-efficient solution.