Vertical ridge augmentation: Using a titanium-reinforced high-density PFTE membrane
Alveolar ridge resorption after tooth extraction is always evident. (1) Most postextraction ridge resorption patterns occur in a horizontal dimension. However, ridge resorption can occur in a vertical dimension under normal conditions or in severe cases under the following clinical situations:
- Long-term removable denture use
- History of severe periodontal or endodontic infection/disease
- History of trauma or neoplasm
- Traumatic tooth extractions
Increasing success rates of short (< 9 mm) (2,3) and extra short (≤ 6mm) (4) dental implants have drastically reduced the need to perform vertical ridge augmentation procedures prior to dental implant therapy. However, there are still many clinical situations that necessitate a vertical ridge augmentation for a successful and esthetic outcome of dental implant therapy.
RELATED |Minimally invasive ridge augmentations
Various types of procedures available for vertical alveolar ridge augmentations include: onlay block grafting (5), distraction osteogenesis (6), guided bone regeneration (GBR) (7), segmental osteotomy/interpositional grafts (8), and titanium mesh grafts with (9) or without(10) rhBMP-2.
RELATED |Is it time to retire the free gingival graft procedure in light of new alternative tissue grafting materials?
All of the mentioned procedures to regenerate a vertically deficient alveolar ridge are extremely technique sensitive and have complications that often occur. Onlay block grafts, even under ideal surgical technique and healing, can suffer from up to 45% volumetric remodeling. This can result in insufficient vertical bone growth. Early graft exposure can also occur resulting in graft failure. Distraction osteogenesis requires frequent visits and a cumbersome distractor to be placed in the patient. Guided bone regeneration, when performed with a titanium-reinforced expanded polytetrafluoroethylene (e-PTFE) membrane and tenting screws, can result in graft infection and failure if the membrane becomes exposed. Segmental osteotomy/interposition grafts can be a risky procedure and result in graft failure if rigid fixation of the segment is not achieved and maintained throughout healing. Titanium mesh grafts can often result in early exposure of the mesh, leading to infection and graft failure.
Most complications during bone grafting are often related to improper surgery techniques and thin soft tissues around the surgical site; therefore, it is often advantageous to perform a soft-tissue augmentation procedure prior to a vertical ridge augmentation in order to ensure thick soft tissues to overly the graft materials, thus minimizing the complication rate.
It is also imperative to follow the basic principles (PASS) of bone regeneration during any ridge augmentation procedure. (11)
- Primary wound coverage and tension-free closure
- Angiogenesis (adequate blood supply and intra-marrow penetrations)
- Space creation/maintenance and exclusion of unwanted cells
- Stability of wound and bone graft
Case example
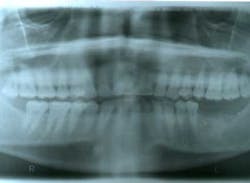
This patient presented with a missing No. 18 and hopeless No. 17 and No. 19 due to localized severe periodontal disease, recurring abscesses, and tooth migration. Severe bone loss can be seen on the initial periapical (Fig. 1) and panoramic (Fig. 2) radiographs.
Fig. 1
Fig. 2
The patient was treatment planned for removal of No. 17 and No. 19 and dental implant replacement for No. 18 and No. 19. Upon removal of the hopeless teeth, a severe vertical and horizontal ridge deficiency will be expected. Teeth No. 17 and No. 19 were removed, the area was thoroughly debrided of granulomatous tissue, and a soft-tissue allograft (perioderm – Dentsply/Tulsa Dental) was placed at the time of tooth removal in order to thicken the soft tissues in preparation for the vertical ridge augmentation procedure.
Approximately eight weeks later, a GBR procedure was done utilizing a vestibular incision approach, reflecting the mucoperiosteal flap beyond the ascending ramus. A combination of FDBA (regeneross, Biomet 3i) and autogenous graft particles harvested from the ascending ramus were placed on the deficient ridge after making cortical perforations. The graft materials were covered with a titanium-reinforced dense polytetrafluoroethylene (d-PTFE) membrane (cytoplast, osteogenics) that was tacked into place in order to maintain graft stability during healing. The membrane extended approximately 2 mm beyond the bone graft materials and was placed up the ascending ramus. Immediately after surgery, a panoramic radiograph was taken (Fig. 3).
Fig. 3
Ten months after the GBR procedure was done, a new panoramic radiograph (Fig. 4) was taken and the site was reentered for implant placement into an ideal restorative position. Dental implants (nobel active 5.0 x 11.5 mm) were placed at the No. 18 and No. 19 positions (Fig. 5), into excellent type I dense bone; note that the majority of the dental implants are completely housed in newly grafted bone. Additional minor bone grafting was done using autogenous coagulum collected during the osteotomies and a xenograft particulate (Bio-Oss, Geistlich), then covered with a resorbable collagen membrane (Biogide, Geistlich) in order to maintain buccal bone stability and contour (Fig. 6). The implants were later uncovered, ensuring that an adequate zone of keratinized tissue was present and the implants were subsequently restored (Figs. 7, 8). The success of this case was dependent upon proper treatment planning, meticulous surgical techniques, patient compliance, and understanding bone and soft-tissue biology.
Fig. 4
Fig. 5
Fig. 6
Fig. 7
Fig. 8
Gregory A. Pette, DMD, MS, is a periodontist and adjunct associate professor in the department of postgraduate periodontics at Nova Southeastern University, Fort Lauderdale, Fla. He also maintains a private practice in periodontics and dental implants in Fort Myers and Miami, Fla. You may contact him by email at [email protected].
References
1. Schropp L, Wenzel A, Kostopoulos L, Karring, T. Bone Healing and Soft Tissue Contour Changes Following Single-Tooth Extraction: A Clinical and Radiographic 12-Month Prospective Study. Int J Periodont Rest Dent. 2003;23:313-323.
2. Annibali S, Cristalli MP, Dell'Aquila D, Bignozzi I, La Monaca G, Pilloni A. Short dental implants: a systematic review. J Dent Res. Jan. 2012;91(1):25-32.
3. Fugazzotto PA. Shorter implants in clinical practice: rationale and treatment results. Int J Oral Maxillofac Implants. May-Jun. 2008;23(3):487-496.
4. Urdaneta RA, Daher S, Leary J, Emanuel KM, Chuang SK. The survival of ultrashort locking-taper implants. Int J Oral Maxillofac Implants. May-Jun. 2012;27(3):644-654.
5. Chiapasco, M., Zaniboni, M. & Rimondini, L. Autogenous onlay bone grafts vs. alveolar distraction osteogenesis for the correction of vertically deficient edentulous ridges: a 2-4-year prospective study on humans. Clin Oral Imp Resh. 2007;18:432-440.
6. McAllister, B. S. Histologic and radiographic evidence of vertical ridge augmentation utilizing distraction osteogenesis: 10 consecutively placed distractors. J Periodontol. 2001;72:1767-1779.
7. Simion, M., Fontana, F., Raperini, G. & Maiorana, C. Vertical ridge augmentation by expanded-polytetrafluoroethylene membrane and a combination of intraoral autogenous bone graft and deproteinized anorganic bovine bone (Bio Oss). Clin Oral Imp Res. 2007:18:620-629.
8. Jensen, O. T., Kuhlke, L., Bedard, J. F. & White, D. Alveolar segmental sandwich osteotomy for anterior maxillary vertical augmentation prior to implant placement. Journal of Oral and Maxillofacial Surgery. 2006;64:290-296.
9. Misch CM. Bone augmentation of the atrophic posterior mandible for dental implants using rhBMP-2 and titanium mesh: clinical technique and early results. Int J Periodontics Restorative Dent. Nov.-Dec. 2011;31(6):581-9.
10. Her S, Kang T, Fien MJ. Titanium mesh as an alternative to a membrane for ridge augmentation. J Oral Maxillofac Surg. Apr. 2012;70(4):803-810.
11. Wang HL, Boyapati L. “PASS” principles for predictable bone regeneration. Implant Dent 2006;15:8-17.