Interdisciplinary management of a complex maxillary implant restoration
Although implants enjoy a high success rate in the literature, the restorative challenge continues to be achieving a desirable result in the maxillary anterior segment. This challenge is further exacerbated by patients presenting with malocclusion, soft tissue loss, hard tissue loss, a high lip line, and/or high esthetic demands. A patient who exhibits all of these factors can only be managed through proper treatment planning. The following case discussion highlights the importance of proper treatment planning and communications that take place between the implant surgeon and restorative dentist.
ALSO BY DR. PETER MANN | Narrow diameter dental implants in the esthetic zone
ALSO BY DR. SCOTT FROUM | Restoration of a damaged dental implant due to removal of a fractured screw: thinking outside the box
A 43-year-old female with a noncontributory medical history taking no medication and having no known food/drug allergies presented to my general dental office with a chief complaint of having “loose teeth with an underbite.” Clinically, she had generalized, moderate, chronic periodontal disease and was missing teeth Nos. 8 through 10. She had a Class III malocclusion with pathologic flaring of her remaining anterior teeth. She had both vertical and horizontal tissue loss in the No. 8 through 10 region. The patient wore a transitional partial denture to replace the anterior missing teeth that was placed in edge-to-edge occlusion by her previous dentist. (Fig. 1) She did not like having a removable prosthetic and desired a fixed option in the form of implants to replace her missing teeth. I sent her to the periodontist for a periodontal consult for her remaining dentition and dental implants to replace her missing front teeth.
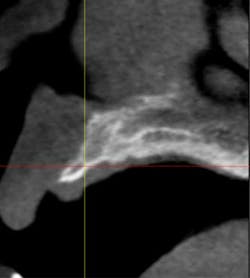
Fig. 2
Fig. 7
Fig. 11
From a restorative perspective, now that the implants were placed in a restoratively driven manner, the main considerations were to address the patient’s malocclusion and correct her edge-to-edge bite while delivering optimal esthetics. In order to accomplish this goal, a framework was fabricated with a wax-up on the casts. (Fig. 14) By utilizing this method at the framework try-in visit, we were able to give the patient an extremely accurate preview of what her final prosthetic would look like.
Fig. 14The patient was satisfied with her overbite, overjet, and overall appearance of the three-unit implant bridge. (Fig. 15). Our final concern was the risk of porcelain fracture due to the patient’s deep bite. She would occlude on the lingual of her new implant bridge with more force than someone with Class I occlusion. By making this prosthesis screw-retained, we will be able to retrieve this bridge in case of future porcelain fracture without destroying the framework. (Fig. 16) We can either repair the porcelain fracture or completely remake the porcelain on top of the existing framework. The lingual, where the patient is occluding, was also left in metal to further reduce the risk of possible porcelain fracture.
Fig. 15
Fig. 17