The free gingival graft (FGG) (Fig. 1) is an age-old periodontal procedure first described by Sullivan & Atkins in 1968. (9) It has long been the gold standard for increasing attached gingiva around the natural dentition. Connective tissue grafting (CTG) (Fig. 2) provides many of the same benefits along with root coverage, without the accompanying discomfort from the donor site, making the FGG less desirable. However, the FGG procedure has its advantages over CTG for both the natural dentition and, more recently, dental implants.
ALSO BY DR. ALBERT YOO |'My implant is too shallow and now I'm getting food stuck between my teeth'
Anatomy(Fig. 3) In a healthy periodontium, there exists the free gingival margin (FGM) along with a zone of attached/keratinized gingiva (AG). The mucogingival junction (MGJ) forms the boundary between the attached tissue and alveolar mucosa (AM), which continues to form the vestibule becoming confluent with the cheek or lip. Literature supports a minimum of 2 mm AG for long-term stability and maintenance. (7) Note: not all keratinized gingiva is attached. The free gingival margin, which forms the external border of the periodontal sulcus, is usually keratinized, but certainly not attached to the underlying bone.
Loss of attached gingiva
Gingival recession is the result of loss of alveolar bone and tissue, specifically AG. A high number of recession cases result in less than the minimum required amount of AG. (Fig. 4) Similarly, following tooth extraction or long-standing edentulism (without bone preservation), loss of alveolar dimension is accompanied with diminishing AG. (Fig. 5)Note: specific cases may also be attributed to gingival biotype and genetic predisposition.
Surgical reconstruction of a deficient ridge/site begins with bone augmentation (i.e., lateral ridge graft, sinus augmentation, etc.), closely followed by soft-tissue augmentation (i.e., onlay graft, pedicle graft, etc.) When either cannot produce adequate ridge form for esthetics, prosthetic solutions are used to compensate for this deficiency. Soft-tissue augmentation, particularly those procedures to increase AG, is often overlooked.
Fig. 6: Implants placed in lateral window sinus graft with no augmentation of attached tissue.
Fig. 7: Failing implants for mandibular overdenture were placed in atrophic mandible with inadequate attached tissue.Comparison
There is an abundance of literature showing increased gingival inflammation around natural dentition (exacerbated when a fixed restoration is present) when there is less than 2 mm AG. (Figs. 8, 9: post grafting) There is an abundance of literature showing increased incidence of peri-implant mucositis when there is inadequate attached tissue — a weaker connective tissue adhesion and lack of Sharpey’s fibers make the peri-implant tissue even more susceptible to bacterial challenge. (1-6, 8, 10) And as periodontitis is always preceded by gingivitis, peri-implantitis will be preceded by peri-implant mucositis. If we can decrease the incidence of peri-implant mucositis by providing a better and more resilient tissue phenotype, we can lower the incidence of peri-implantitis.The FGG procedure is indicated in cases of implant therapy where this is less than 2 mm of attached tissue present. Sometimes, a FGG is preferred over CTG because: (1) the FGG results in greater gain of attached tissue, (2) the FGG alleviates frenum/muscular pull whereas the connective tissue may increase muscular tension after the flap is coronally advanced, and (3) creeping attachment is often a positive byproduct of the FGG procedure.
Refer to Case Nos. 1 & 2.
Case No. 1
Case No. 2
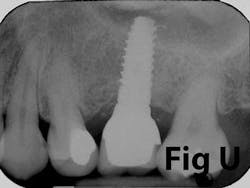
Fig. U: Final radiograph (six-months post-placement) demonstrating excellent bone level.
References
1. Adibrad M, Shahabuei M, Sahabi M. Significance of the width of keratinized mucosa on the health status of the supporting tissue around implants supporting overdentures. J Oral Implantol.2009;35(5):232-237.
2. Artzi Z, Tal H, Moses O, Kozlovsky A. Mucosal considerations for osseointegrated implants. J Prosthet Dent. Nov. 1993;70(5):427-432.
3. Bouri A Jr, Bissada N, Al-Zahrani MS, Faddoul F, Nouneh I. Width of keratinized gingiva and the health status of the supporting tissues around dental implants. Int J Oral Maxillofac Implants. Mar.-Apr. 2008;23(2):323-326.
4. Boynuegri D, Nemli SK, Kasko YA. Significance of keratinized mucosa around dental implants: a prospective comparative study. Clin Oral Implants Res. Aug. 2013;24(8):928-933.
5. Chung DM, Oh TJ, Shotwell JL, Misch CE, Wang HL. Significance of keratinized mucosa in maintenance of dental implants with different surfaces. J Periodontol. Aug. 2006;77(8):1410-1420.
6. Kim BS, Kim YK, Yun PY, Yi YJ, Lee HJ, Kim SG, Son JS. Evaluation of peri-implant tissue response according to the presence of keratinized mucosa. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. Mar. 2009;107(3).
7. Lang, N.P. & Loe, H. The relationship between the width of keratinized gingiva and gingival health. Journal of Periodontology 43;623-627.
8. Schrott AR, Jimenez M, Hwang JW, Fiorellini J, Weber HP. Five-year evaluation of the influence of keratinized mucosa on peri-implant soft-tissue health and stability around implants supporting full-arch mandibular fixed prostheses. Clin Oral Implants Res. Oct. 2009;20(10):1170- 1177.
9. Sullivan H., Atkins J. Free Autogenous Grafts. I. Principals of successful grafting. Periodontics 1968; 6(1) 5-13.
10. Warrer K, Buser D, Lang NP, Karring T. Plaque-induced peri-implantitis in the presence or absence of keratinized mucosa. An experimental study in monkeys. Clin Oral Implants Res. Sept. 1995;6(3):131-138.
Albert Yoo, DDS, completed his predoctoral training at the Stony Brook School of Dental Medicine in 2005. He received his certificate in periodontics and implantology in Stony Brook in 2008. He is in full-time private practice and has lectured to numerous study clubs, with special interest in perio-prosthetics, advanced bone grafting, and sinus lift procedures, and immediate implant placement. He is a clinical assistant professor in the Department of Periodontics at Newark Beth Israel Hospital, Stony Brook School of Dental Medicine, and New York Hospital of Queens. He maintains a private practice in Bayside, N.Y.