Hyperparathyroidism-jaw tumor syndrome (HPT-JT): report of a family
The hyperparathyroidism-jaw tumor syndrome (HPT-JT) is an autosomal dominantly inherited disorder whose principal features are neoplastic and/or cystic lesions in three main organs: the parathyroid glands, the jaws, and the kidneys.Correctly diagnosingHPT-JT syndrome is essential because of the possible involvement of other family members and risk of malignant disease. The jaw tumors, which can involve the maxilla or mandible, can be bilateral or recurrent lesions. Microscopically, the jaw tumors are cemento-ossifying fibroma.
The syndrome was first documented by Jackson (1958), who reported multiple cases of primary hyperparathyroidism (PHPT) and jaw tumors in three generations of the same family. Histologically, the jaw tumors were described as benign fibro-osseous lesions without giant cells. Reports of several additional kindreds have improved our understanding of the disease-associated phenotypes.
Parathyroid malignancy, an otherwise rare cause of PHPT,is recognized in approximately a third of patients. In a subset of the patients, renal lesions are identified and include hamartomas, renal cysts, polycystic kidney disease, and Wilm’s tumor. Linkage analysis assigned the disease-predisposing geneHRPT2to the long arm of chromosome 1 at the q21-q31 region. The HRPT2 gene encodes a 531 aa tumor suppressor termed parafibromin. The presence of multiple cemento-ossifying fibromas and/or the presence of more than one family member should prompt consideration of the possibility of the syndrome.
Case report
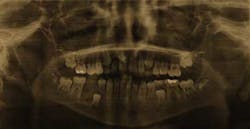
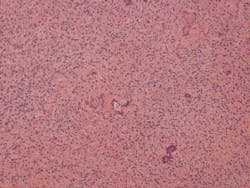
In June 2010, a healthy 9-year-old male presented to an oral and maxillofacial surgeon for evaluation of a lesion of right mandible No. 29 area. Panoramic radiograph Fig. 1revealed a mixed radiolucent radiopaque lesion in the area of missing tooth T and overlying the crown of developing tooth No. 29. Curettage of the area was performed and the tissue was placed in formalin and sent to the oral and maxillofacial pathology laboratory at The Mount Sinai Hospital in New York City.Fig. 1: Panoramic radiograph of a 9-year-old male reveals a mixed radiolucent — radiopaque lesion of the right mandible in the area of missing tooth T and overlying the crown of developing tooth No. 29.Fig. 2 demonstrates a fibrocollagneous cellular stroma containing scattered, small basophilic calcifications. A diagnosis of benign fibro-osseous lesion was made, and after radiographic correlation cemento-ossifying fibroma of bone was added to the final diagnosis.
Fig. 2: Hematoxylin and Eosin stained slide of cemento-ossifying fibroma of bone removed from the right mandible in a 9-year-old male.After receiving the final pathology report, the oral and maxillofacial surgeon called the oral pathology laboratory to notify the lab that the mother of the child had bilateral cemento-ossifying fibromas of mandible that were removed one year prior in 2009. (Figs. 3 and 4)
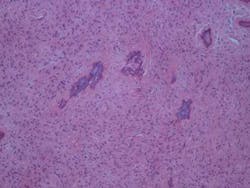
Fig. 3: Hematoxylin and Eosin stained slide of cemento-ossifying fibroma of bone involving the right mandible in the patient’s 35-year-old mother.
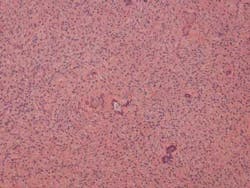
Fig. 4: Hematoxylin and Eosin stained slide of cemento-ossifying fibroma of bone involving the left mandible in the patient’s 35-year-old mother.
In December 2010, the patient returned to the oral and maxillofacial surgeon, and panoramic radiograph revealed a recurrence of the tumor. The lesion was excised, and the tissue was placed in formalin and sent to the oral pathology laboratory. The histology of the first recurrence was identical to the initial surgical specimen as well as the bilateral tumors of the patient’s mother.
In January 2012, the 10-year-old patient returned to the oral and maxillofacial surgeon with swelling of the right face. Radiographic cone beam computed tomography Fig. 5revealed the second recurrence of the tumor.Fig. 5: Radiograph of right mandible depicts the second recurrence of a cemento-ossifying fibroma of bone in a 10-year-old male with hyperparathyroidism-jaw tumor syndrome.
The patient was referred to Mount Sinai Hospital Department of Oral and Maxillofacial Surgery for surgical resection of the tumor and simultaneous reconstruction utilizing a reconstruction plate. Genetic testing of serum and histologic paraffin fixed tissue blocks of both the mother and her 10-year-old son were performed and mutations of HRPT2 gene were found, thus confirming the diagnosis of hyperparathyroidism-jaw tumor syndrome in a child and his mother.