Dismay with kid decay: treatment options for broken down permanent teeth in the mixed dentition
Introduction
Management of cariously involved and traumatized permanent teeth in the mixed dentition depends on many factors. This article will seek to identify the factors involved in the treatment planning of permanent dentition that require root canal therapy due to trauma or caries.
Immature permanent dentition requiring endodontic intervention can be researched by following the lifetime work of Jens Ove Andreasen or by reading the landmark research of Mejare Cvek and are beyond the scope of this review. Of principal concern in the management is the mean time to permanent restoration. In general, the permanent restoration is desired after full growth of the individual. Individual growth can be measured by taking a hand wrist film (1) or two consecutive cephalometric radiographs that confirm no further dental growth is seen. (2,3)
ALSO BY DRS. DIBERNARDO AND TOSKOS |Endodontic therapy vs. implant maintenance: an evidence-based review
When considering a candidate for dental restoration, the first step is to determine the etiology of the disease. If dental caries is determined to be the primary cause of necessary endodontic intervention, the individual and guardian must be educated about the etiology of dental decay. (4) Dietary modification, oral hygiene instruction, and topical or systemic flouride therapy where indicated are necessary in the further prevention of the disease. (5) Sealant therapy on at-risk teeth should be treatment planned. (5) Orthodontic considerations that impede proper hygiene and serve as food entrapment should be considered as well. (6)
Dental trauma to the anterior teeth is not a predictable event. Orthodontic malposition of the teeth, such as flared anterior teeth, can be a strong risk factor for dental trauma, (7) after which corrective dental appliances can be used as habit-breaking devices to stop the pathological behavior. (8) If the malposition can be corrected with interceptive orthodontic procedures, this may be beneficial in preventing future trauma to the anterior teeth. (9) The guardian and child should also be educated about the benefits of protective appliances for use in contact sports and physical educational activities, although the evidence for the protective benefits of these appliances is weak. (10,11)
ALSO BY DRS. DIBERNARDO AND TOSKOS | To retreat or not: a decision matrix
If the tooth is deemed salvageable, then the tooth may be transitionally restored with a core buildup and stainless steel crown following endodontic therapy or a composite restoration for anterior teeth with a resin-based crown if necessary. (12,13,14) The treatment plan should involve long-range case management that will include conversion to final fixed prosthetics at the time that growth ceases and orthodontic treatment is finished. (2,3)
If the tooth is deemed nonrestorable, then case management does become increasingly more complex. The ultimate desire is to maintain as much cortical and cancellous bone as possible with the ultimate definitive treatment being dental implant placement. (15,16) Implant placement may be delayed for long periods of time, and full growth of the individual may not occur for as many as 15 years depending upon the age of trauma of the child’s growth. Single tooth loss can bring on significant restorative challenges when the child transitions to full adult dentition, including lost vertical bone height and horizontal width, compromising the placement of the dental implant and causing esthetic issues that will not be easily overcome. (17,18)
Inability or failure to manage the edentulous space could lead to significant occlusal issues that may be difficult or impossible to manage and may lead to compromised fixed prosthetics in the adult dentition, causing further dental issues over the individual’s lifetime. (19,20) The treatment options for a compromised, nonrestorable tooth may include the decorination of the existing tooth fragments followed by endodontic treatment. (21) A tissue-friendly restoration of Geristore could serve as a temporary and transitional restoration of the root fragment as the root structure serves to maintain bone. (21,22) If possible, a bonded Maryland bridge could be placed to maintain the space and prevent posterior tooth tipping. (23,24) A space maintainer, Maryland bridge, or removable appliance should be considered in the missing anterior tooth. (21) Oftentimes, traumatized anterior dentition occurs about or around the time of orthodontic intervention. A Hawley appliance can be constructed with a prosthetic tooth bonded to the arch wire and worn by the preteen until banded orthodontic therapy begins, at which time a denture tooth could be bonded to the arch wire.
The following case was treated in clinical practice with the intention of retaining bone for future implant placement.
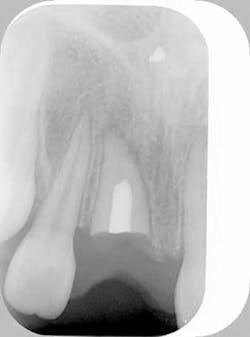
Case study — Traumatized anterior tooth (root submersion case)Fig. 1a: Initial radiograph of a traumatized tooth No. 8 in a female patient too young for dental implants
Fig. 1b: Clinical presentation of the traumatized tooth
Fig. 2a: Post endodontic treated tooth prepared for decorination and root submersion for the purposes of preservation of alveolar bone prior to implant therapy
Fig. 2b: Clinical smile of patient with orthodontic appliance to replace decorinated tooth
Fig. 2c: Hawley appliance inserted with pontic in the No. 8 region
Doreen Toskos, DMD, was raised on Long Island. Following her undergraduate studies at Cornell University, Dr. Toskos received her DMD degree from Harvard University in Boston, Mass. She then returned to New York for a two-year postgraduate residency in endodontics at Columbia University. Since the completion of her training, Dr. Toskos has practiced on Long Island and lectured for general dentists and the New York Dental Association. She stays actively involved in continuing education. She is an attending endodontist for the general practice and pediatric residency programs at Brookdale Hospital.
Joseph F. DiBernardo, DDS, was raised on the north shore of Long Island. He obtained both his undergraduate and dental degrees from Stony Brook University. After his dental school training, he completed a general practice residency program at Nassau University Medical Center. He has worked as a general dentist for three years, both in Long Island and New Jersey. He returned to New York to complete a two-year residency program to specialize in endodontics at New York University in Manhattan. He then returned to Long Island to establish Smithtown Endodontics. Dr. DiBernardo is on staff at the general practice residency program at Stony Brook University Dental School.
References
1. Flores-Mir C, Nebbe B, Major PW. Use of skeletal maturation based on hand-wrist radiographic analysis as a predictor of facial growth: a systematic review. Angle Orthod. Feb. 2004;74(1):118-124.
2. Durka-Zając M, Marcinkowska A, Mituś-Kenig M. Bone age assessment using cephalometric photographs. Pol J Radiol. Apr. 2013;78(2):19-25. doi: 10.12659/PJR.889072.
3. Subramaniam P, Naidu P. Mandibular dimensional changes and skeletal maturity. Contemp Clin Dent. Oct. 2010;1(4):218-222. doi: 10.4103/0976-237X.76387.
4. Bánóczy J, Rugg-Gunn A. Epidemiology and prevention of dental caries. Acta Med Acad. Nov. 2013;42(2):105-107.
5. Rugg-Gunn A. Dental caries: Strategies to control this preventable disease. Acta Med Acad. Nov. 2013;42(2):117-130. doi: 10.5644/ama2006-124.80.
6. Feliu JL. Long-term benefits of orthodontic treatment on oral hygiene. Am J Orthod. Dec. 1982;82(6):473-477.
7. Prabhu A, Rao AP, Govindarajan M, Reddy V, Krishnakumar R, Kaliyamoorthy S. Attributes of dental trauma in a school population with active sports involvement. Asian J Sports Med. Sep. 2013;4(3):190-194. Epub Mar. 29, 2013.
8. Onyeaso CO, Denloye OO, Taiwo JO. Preventive and interceptive orthodontic demand for malocclusion. Afr J Med Med Sci. Mar. 2003;32(1):1-5.
9. Borrie F, Bearn D. Interceptive orthodontics--current evidence-based best practice. Dent Update. Jul.-Aug. 2013;40(6):442-444, 446-448, 450.
10. Sigurdsson A. Evidence-based review of prevention of dental injuries. Pediatr Dent. Mar.-Apr. 2013;35(2):184-190.
11. Ozawa T, Takeda T, Ishigami K, Narimatsu K, Hasegawa K, Nakajima K, Noh K. Shock absorption ability of mouthguard against forceful, traumatic mandibular closure. Dent Traumatol. Sep. 2, 2013. doi: 10.1111/edt.12063. [Epub ahead of print]
12. Dammaschke T, Nykiel K, Sagheri D, Schäfer E. Influence of coronal restorations on the fracture resistance of root canal-treated premolar and molar teeth: a retrospective study. Aust Endod J. Aug. 2013;39(2):48-56. doi: 10.1111/aej.12002. Epub Dec. 12, 2012.
13. Cohen-Carneiro F, Sponchiado EC Jr, Garcia Ldo F, Yurtsever FV, Pontes DG, Sena A.
Author information Coronal reconstruction following anterior teeth traumatism: multidisciplinary treatment. Gen Dent. Aug. 2013;61(5):47-49.
14. Hutcheson C, Seale NS, McWhorter A, Kerins C, Wright J. Multi-surface composite vs. stainless steel crown restorations after mineral trioxide aggregate pulpotomy: a randomized controlled trial. Pediatr Dent. Nov.-Dec. 2012;34(7):460-467.
15. van Kesteren CJ, Schoolfield J, West J, Oates T. A prospective randomized clinical study of changes in soft tissue position following immediate and delayed implant placement. Int J Oral Maxillofac Implants. May-Jun. 2010;25(3):562-570.
16 [Article in Hebrew] Levin I, Ashkenazi M, Schwartz-Arad D. [Preservation of alveolar bone of un-restorable traumatized maxillary incisors for future]. Refuat Hapeh Vehashinayim. Jan. 2004;21(1):54-59, 101-102.
17. Bahat O, Sullivan RM, Smidt A. Placement of Brånemark Mk IV implants in compromised and grafted bone: radiographic outcome of 61 sites in 27 patients with 3- to 7-year follow-ups. Quintessence Int. Apr. 2012;43(4):293-303.
18. Bidra AS, Chapokas AR. Treatment planning challenges in the maxillary anterior region consequent to severe loss of buccal bone. J Esthet Restor Dent. Dec. 2011;23(6):354-360. doi: 10.1111/j.1708-8240.2011.00475.x. Epub Sep. 20, 2011.
19. [Article in Chinese] Dai LX, Tong WL, Guo JL. [The role of occlusal factors in the occurrence of vertical root fracture]. Shanghai Kou Qiang Yi Xue. Feb. 2013;22(1):68-71.
20. Craddock HL. Occlusal changes following posterior tooth loss in adults. Part 3. A study of clinical parameters associated with the presence of occlusal interferences following posterior tooth loss. . J Prosthodont. Jan. 2008;17(1):25-30. Epub Oct. 8, 2007.
21. Lin S, Schwarz-Arad D, Ashkenazi M. Alveolar bone width preservation after decoronation of ankylosed anterior incisors. J Endod. Dec. 2013;39(12):1542-1544. doi: 10.1016/j.joen.2013.08.003. Epub Sep. 18, 2013.
22. Gupta SK, Saxena P, Pant VA, Pant AB. Adhesion and biologic behavior of human periodontal fibroblast cells to resin ionomer Geristore: a comparative analysis. Dent Traumatol. Oct. 2013;29(5):389-93. doi: 10.1111/edt.12016. Epub Nov. 6, 2012.
23. Sailer I, Bonani T, Brodbeck U, Hämmerle CH. Retrospective clinical study of single-retainer cantilever anterior and posterior glass-ceramic resin-bonded fixeddental prostheses at a mean follow-up of 6 years. Int J Prosthodont. Sep.-Oct. 2013;26(5):443-450. doi: 10.11607/ijp.3368.
24. Ozcan M, Breuklander M, Salihoglu-Yener E. Fracture resistance of direct inlay-retained adhesive bridges: effect of pontic material and occlusal morphology. Dent Mater J. 2012;31(4):514-522.